New Care Pathways Successfully Reduce Opioid Usage for Benign, Malignant Urology Patients
In 2018, Pennsylvania providers wrote 49.9 opioid prescriptions for every 100 persons, slightly lower than the average U.S. rate of 51.4 prescriptions. Yet opioids still accounted for a record 2,866 fatalities (roughly 65% of all drug overdose deaths) statewide.
These troubling trends inspired two urologists from Penn State Health Milton S. Hershey Medical Center to revise care pathways—one for urologic cancer patients, the other for symptomatic nephrolithiasis (kidney stone) patients—with encouraging results. The Milton S. Hershey Medical Center has decreased patient dependence on morphine milligram equivalents (MME) medications by 86% over the past 18 months.
Dr. Jay Raman’s inspiration to change the pathways began when he reviewed a study of U.S. military veterans that explored risk factors for opioid misuse among cancer patients. The study followed 106,732 cancer survivors and found an overall incidence of persistent posttreatment opioid use of 8.3%. Opioid-naïve patients who received opioids during the diagnostic and treatment period reported a 6.2% rate of persistent post-treatment opioid use compared with 1.5% of those who did not receive a prescription. “It was eye-opening to see that, while doctors were curing their cancer, they were leaving them with a lifelong dependence in some cases,” Raman said.
Raman pulled together a Hershey Medical Center team—including urologic surgeons, nurse practitioners, nurses, neurologists, anesthesiologists and oncologists—to redefine the pathway for cancer patients. Simultaneously, Dr. Necole Streeper worked with a team to redefine the pathway for symptomatic nephrolithiasis patients. “Because kidney stones are often recurrent, we see some patients over many years,” Streeper said. “Many of these patients see different physicians during an acute episode and therefore run significant risk of being overprescribed opioids.”
To reduce that risk, Streeper’s team first conducted an Institutional Review Board-approved six-month retrospective review (May – October 2017), comparing data from the hospital’s electronic medical record (EMR) and the Pennsylvania Prescription Drug Monitoring Program (PDMP) database, which collects information on all controlled substances prescribed statewide.
“We found that, despite the integration of PDMP into our EMR, in 20% of cases, we prescribed opioids for kidney stone patients, not knowing they had received opioid prescriptions from other providers,” Streeper said. “This emphasized that there is still work to be done to reduce opioid overprescribing.”
The new pathways begin with frank conversations between providers and patients. Providers perform a thorough review of a patient’s current medications and check the EMR and PDMP database to help identify whether a patient has a prior opioid prescription. Providers then set expectations, letting patients know that while providers will do their best to keep pain controlled with non-opioids, they likely will experience some discomfort after the procedure or while passing a kidney stone.
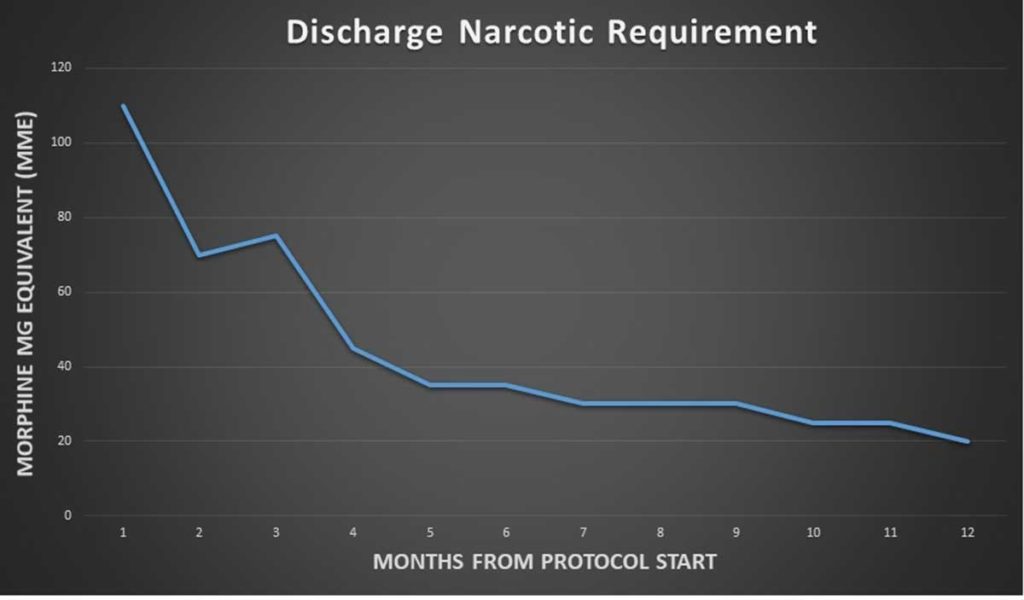
Steep reduction in the requirement of morphine milligram equivalents (MME) one year from protocol start.
Instead of routinely providing narcotic pain medication to all patients as was done previously, Hershey Medical Center providers now use a new algorithm that emphasizes non-narcotic pain medications. Postoperative surgical patients receive acetaminophen, gabapentin, IV ketorolac and ibuprofen as a matter of course. If pain persists above the pain level of 5 to 7 or 8 to 10 on a Likert scale, a weaker opioid (such as 50 mg or 100 mg of tramadol) is initiated. Stronger opioids such as oxycodone, dilaudid or morphine are to be used only if absolutely necessary.
Upon discharge, patients are prescribed acetaminophen, gabapentin and ibuprofen. Tramadol and oxycodone are provided for home use in small amounts (10 pills each) only if ordered postoperatively. “We won’t necessarily prescribe opioids to patients unless we know they are being properly medicated with non-opioid medications and still having significant breakthrough pain,” Raman said.
Providers tracked the number of MMEs Hershey Medical Center patients were filling 30 days post-surgery to measure the new protocols’ efficacy. In the first month, the average patient was receiving more than 100 MMEs 30 days after surgery. At month 18, that number reduced to 14 MMEs at 30 days.
“The data is clear that we’re in the midst of an opioid epidemic,” Raman said. “We encourage practitioners to look at their own practices and think about what changes they can make to reduce opioid prescribing. Even small modifications can make a big difference.”

Jay D. Raman, MD
Chair, Department of Urology
Professor, Department of Urology
Professor, Department of Surgery, Penn State Cancer Institute
Head, Robotic Surgery
Phone: 717-531-8887
Email: jraman@pennstatehealth.psu.edu
Fellowship: Urology, University of Texas Southwestern Medical Center, Dallas
Residency: General Surgery, New York-Presbyterian Weill Cornell Medical Center, New York; Urology, New York-Presbyterian Weill Cornell Medical Center, New York
Medical School: Weill Cornell Medicine/Cornell University, New York
Connect with Jay D. Raman, MD, on Doximity

Necole M. Streeper, MD
Associate professor, Department of Urology, Penn State Health Milton S. Hershey Medical Center
Phone: 717-531-8849
Email: nstreeper@pennstatehealth.psu.edu
Fellowship: University of Wisconsin Hospitals and Clinics, Madison, WI
Residency: University of Texas Health Sciences Center, San Antonio, Texas
Medical School: University of Iowa College of Medicine, Iowa City, IA
Connect with Necole M. Streeper, MD, on Doximity
References:
- National Institute on Drug Abuse – https://www.drugabuse.gov/drug-topics/opioids/opioid-summaries-by-state/pennsylvania-opioid-involved-deaths-related-harms#:~:text=In%20Pennsylvania%2C%2065%25%20of%20drug,did%20not%20meet%20inclusion%20criteria. – Accessed: April 3, 2020
- Predicting Persistent Opioid Use, Abuse, and Toxicity Among Cancer Survivors – https://academic.oup.com/jnci/article/112/7/720/5618684 – Accessed: November 20, 2019
