Penn State Health Offers Latest Innovations in Benign Prostatic Hyperplasia Treatment
The surgical urology team at Penn State Health Milton S. Hershey Medical Center offers the full range of minimally invasive and surgical treatments for benign prostatic hyperplasia (BPH), a noncancerous enlargement of the prostate gland experienced by many men. The condition affects approximately half of men by midlife, according to the Urology Care Foundation. Up to 90% of men over age 80 will have BPH.
A walnut-shaped gland that produces fluid in semen, the prostate wraps around the urethra, the tube that transports urine out of the bladder. In BPH, the enlarged prostate compresses the urethra, interfering with urine flow. The bladder becomes overworked and may eventually weaken. These changes can cause urination problems, including increased frequency or urgency, a delayed, interrupted or weak stream or urinary retention or incontinence. As the bladder retains urine, complications such as stones or infections can also occur.
Initially, patients may simply be watched for worsening symptoms if their condition is not overly bothersome, according to Dr. Jeffrey L. Rosenblum, an assistant professor in the Department of Urology at Penn State College of Medicine. They may be advised to make lifestyle changes, such as limiting liquids before sleep or cutting back on caffeine or alcohol.
Medications to relax or shrink the prostate, such as alpha blockers, 5-alpha reductase inhibitors or a combination, are the first line of treatment for BPH. However, in some patients the medications aren’t effective or can lose their effectiveness over time. Patients may also experience side effects such as low blood pressure, dizziness or decreased libido with the drugs.
In these patients, a minimally invasive procedure or surgery may be warranted. Decades ago, before medications and less invasive procedures for BPH, surgeons made an incision into the pelvis and manually removed excess prostate tissue. Today, most BPH procedures are far less invasive and are performed with transurethral approach, in which a device is inserted through the penis and urethra to reach the prostate. No incision is made on the outside of the body.
Urologists at Penn State Health may use one of these treatments, depending on the patient’s individual case:
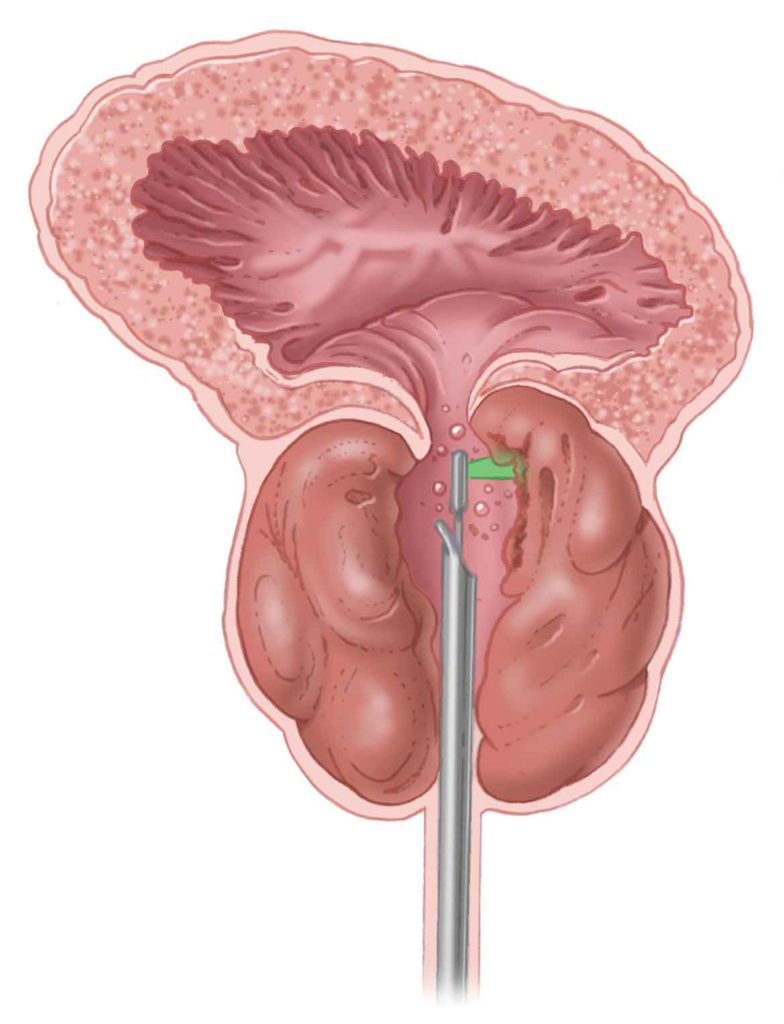
The GreenLight laser procedure permits vaporization of prostate tissue to create a channel, improving urine flow. The image shows the prostate during treatment.
Transurethral resection of the prostate (TURP) has been the gold-standard surgery for BPH. In this procedure, an electrical cautery loop shaves chips off the inside of the prostate gland. The tissue pieces are carried in fluid to the bladder and then flushed out. The TURP procedure requires general or spinal anesthesia and at least a one-night hospital stay, with catheterization for several days after the procedure.
Although TURP has been the most common procedure performed for BPH, other minimally invasive procedures offered at Penn State Health are also gaining in popularity due to promising results with lower potential morbidity.
Dr. John J. Knoedler, an assistant professor in the Department of Urology at Penn State College of Medicine, performs the Holmium Laser Enucleation of Prostate (HoLEP) procedure, in which a laser is used to remove overgrown tissue from the prostate. The tissue fragments are pushed into the bladder, where they are morcellated by a device prior to being evacuated.
The HoLEP procedure can be used for an enlarged prostate of any size, but it’s among the best choice for exceptionally large prostate glands that weigh more than 80 grams. The technique has a low likelihood of postprocedural bleeding (1%), making it a good option for patients who take anticoagulant medications or who have bleeding disorders.
HoLEP can be performed in an outpatient setting or can require an overnight stay. It removes more excess prostate tissue than other procedures, giving it the lowest reoperation rate. “The odds of needing to go for another surgery or go back on medication in someone’s lifetime is about 1% to 2% after a HoLEP,” Dr. Knoedler said. “So if someone’s looking for the most definitive option, it’s the most likely to be a one-and-done.”
GreenLight Laser therapy is another laser treatment for BPH offered at Penn State Health. Dr. Rosenblum is one of few surgeons in the region surrounding Penn State Health who performs the procedure, in which high-powered green light laser pulses are aimed at excess prostate tissue. Red blood cells in the tissue absorb the light and heat up, causing the tissue to vaporize. The vapor is then irrigated from the bladder.
The technique—also known as photoselective vaporization of the prostate, or PVP—seals off the blood vessels, resulting in low rates of bleeding. Dr. Rosenblum uses the latest generation GreenLight Laser device, which is notable for improvements in the laser technology. These advances allow superior vaporization and hemostasis of tissue in a shorter amount of operative time. Most patients undergoing the procedure go home the same day.
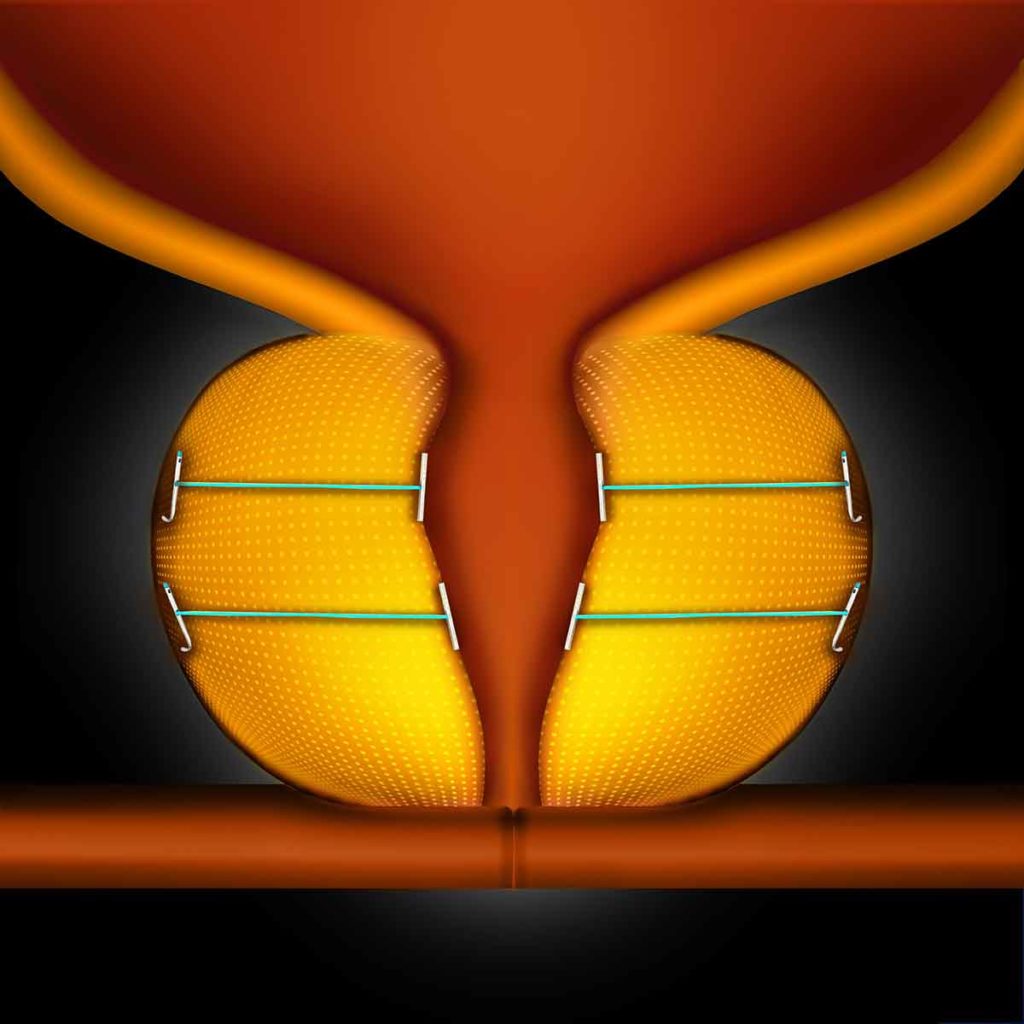
The UroLift System is a relatively simple procedure that utilizes tiny implants to lift and hold the enlarged prostate tissue out of the way so it no longer blocks the urethra.
Dr. Joseph Y. Clark, an associate professor in the Department of Urology at Penn State College of Medicine, performs one of the newest minimally invasive techniques for BPH, the UroLift System. In this quick outpatient procedure, small implants are inserted to hold the prostate lobes open, making more room for urine to flow through the urethra. The technique is appropriate for men with BPH symptoms who have prostate glands smaller than 80 grams. Because it takes less than hour, the procedure may be recommended for patients for whom longer sedation is a concern.
One of the greatest benefits of the UroLift is the limited side effects following the procedure. After a TURP or HoLEP, most patients experience retrograde ejaculation—or dry orgasms. Additionally, at least a third of patients experience dry orgasms with the GreenLight Laser procedure. Conversely, the UroLift procedure preserves both erectile and ejaculatory function.
Recently, the indications for using the UroLift System were expanded to include men younger than 45 years old, as well as those with enlarged median prostate lobes. (It was previously approved for use only in older men with enlarged lateral prostate lobes.) Although the UroLift is the least invasive of BPH procedures, symptoms and flow rate improve more with TURP. In clinical studies, the UroLift procedure has been proven to be safe and effective in patients for five years. An advantage of the procedure is that it does not rule out other treatment options such as the GreenLight Laser, HoLEP, or TURP if needed down the line, Dr. Clark said.
For all these BPH procedures, the recovery period can range from a few days to a few weeks, with the UroLift often having the shortest recovery.
The right procedure for an individual patient will depend on his urologist’s experience as well as factors like the patient’s age, prostate size and anatomy, level of symptom severity and comorbidities. Urologists at Penn State Health are trained in the full spectrum of procedures to treat men with BPH symptoms requiring surgery.

Jeffrey L. Rosenblum, MD
Assistant Professor, Department of Urology, Penn State College of Medicine
Phone: 717-715-1001
Email: jrosenblum@pennstatehealth.psu.edu
Residency: Urology, New York University Medical Center, New York; General Surgery, New York University Medical Center, New York; General Surgery, Bellevue Hospital Center, New York University, New York
Medical School: Boston University School of Medicine, Mass.
Connect with Jeffrey L. Rosenblum, MD, on Doximity

John J. Knoedler, MD
Assistant Professor, Department of Urology, Penn State College of Medicine
Phone: 717-531-8887
Email: jknoedler@pennstatehealth.psu.edu
Fellowship: Minimally Invasive Urologic Surgery, Mayo Graduate School of Medicine, Minnesota
Residency: Urology, Mayo Graduate School of Medicine, Minnesota
Medical School: Penn State College of Medicine, Hershey, Pa.
Internship: General Surgery, Mayo Graduate School of Medicine, Minnesota
Connect with John J. Knoedler, MD, on Doximity

Joseph Y. Clark, MD
Associate Professor, Department of Urology, Penn State College of Medicine
Phone: 717-531-8887
Email: jclark13@pennstatehealth.psu.edu
Fellowship: Urologic Oncology, National Cancer Institute – Bethesda, Md.
Residency: Urology, Wilford Hall Medical Center, Texas
Medical School: Uniformed Services University of the Health Sciences
Internship: Transitional, Madigan Army Medical Center, Washington
Connect with Joseph Y. Clark, MD, on Doximity
Reference:
What is Benign Prostatic Hyperplasia (BPH)? Urology Care Foundation. https://www.urologyhealth.org/urologic-conditions/benign-prostatic-hyperplasia-(bph). Updated May 2019.
