Complex Limb Reconstruction Case Report: Combined Use of the Ilizarov Technique and Taylor Spatial Frame
Successful combined use of the Ilizarov technique and Taylor spatial frame spared a healthy mother of two from the amputation of her left leg (above the knee) following a traumatic accident; the team was able to save her knee and work to heal it before any amputation needed to occur. According to J. Spence Reid, MD, trauma surgeon, Penn State Bone and Joint Institute, “An initial attempt to reconstruct the knee failed when massive infection developed. Debridement of infected tissue and bone resulted in large bone defects.” Reid and the patient discussed amputation versus preserving the limb. “As an active young woman, the patient and her family felt very strongly about trying to preserve the leg.” Thankfully there were options.
After enduring six months of the Ilizarov and Taylor spatial frame techniques, and eight surgeries in 12 months, including fusion of the knee and placement of an intermedullary nail, the bone defects have fully healed and the patient is able to walk and perform most normal daily activities with no pain or ambulatory aids. Reid adds, “This was a highly personal decision to undergo an arduous, painful, and expensive series of treatments. While this approach is not for everyone, the patient and her family are very satisfied with the outcome.”
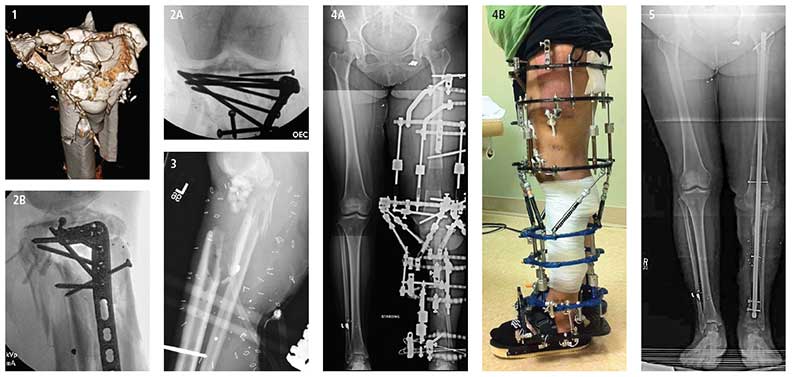
FIGURE 1: Patient is a healthy female; mother of two. Three-dimensional CT scan shows highly comminuted traumatic injury to left proximal tibia.
FIGURES 2A and B: Following multiple debridements, an attempt was made to reconstruct the proximal tibia and close the wound.
FIGURE 3: Massive post-operative infection led to removal of all infected hardware, soft tissue and bone; bone defects totaled 11 centimeters. Antibiotic beads were placed into the wound area.
FIGURES 4 and B: The Ilizarov technique and Taylor spatial frame were used for six months to heal the bone defects; the left knee joint was fused, resulting in a non-bending knee.
FIGURE 5: An intermedullary nail was passed down through the bone for the final stage of bone-defect healing. The patient has recovered well with no pain, no use of ambulatory aids, and was able to resume most activities of daily living, including driving. Stair climbing and certain sitting situations remain a challenge.
J. Spence Reid, MD
Orthopaedic Surgeon, Trauma
Professor, Orthopaedics and Rehabilitation
Phone: 717-531-1363
Email: jreid@pennstatehealth.psu.edu
Fellowship: Orthopaedic trauma, R. Adams Cowley Shock Trauma Center, Baltimore, Maryland
Residency: Orthopaedic surgery, Penn State Health Milton S. Hershey Medical Center, Hershey, Pa.
Medical School: Penn State College of Medicine, Hershey, Pa.
Connect with Penn State Bone and Joint Institute on Doximity
