Cervical Radiculopathy: Cervical Disc Arthroplasty versus Fusion
For patients with cervical radiculopathy, total disc replacement using artificial disc devices that have become more widely used during the last 10 years presents a potential advance in treatment. It may preserve range-of-motion and decrease the need for later secondary surgery when compared to the standard anterior discectomy and spinal fusion. “Artificial disc devices can yield good results in the right patients,” notes Mark Knaub, MD, assistant professor and associate director of the Penn State Spine Center. However, Dr. Knaub explains that there are significant limitations to their usefulness: “These devices are not appropriate to use in patients with poor bone quality or disc disease affecting multiple levels, nor for patients with a pre-existing fusion, those who present with significant arthritis and those with already limited range-of-motion.” While clinical trials show improvement of symptoms with disc arthroplasty,1,2 there is controversy regarding whether a cervical disc arthroplasty can reduce the frequency of reoperations, compared with fusion.
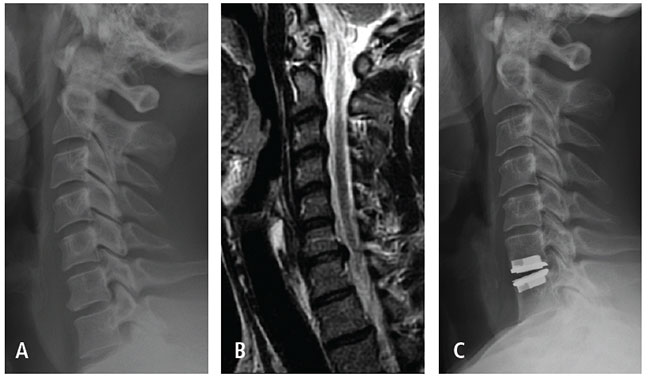
Patient is a healthy, active 40-year-old male with history of radiating right arm pain in a C7 nerve root distribution. He failed conservative treatment.
(A) Pre-operative X-ray shows mild spondylosis at C6-7 with preserved disc height.
(B) Pre-operative MRI shows a foraminal disc herniation at C6-7. Patient chose to undergo anterior cervical discectomy and disc replacement at C6-7 with complete relief of his right arm symptoms.
(C) Follow-up X-ray at 2.5 years after surgery shows no evidence of device-related complications.
Dr. Knaub says, “Patients who are good candidates for an artificial disc tend to be younger, healthier and more active. Mid- to long-term outcomes are encouraging and I’m cautiously optimistic about their usefulness.” According to published findings of large systematic meta-analyses,3,4 patients who underwent cervical disc arthroplasty with either an artificial disc placed at a single level or two disc devices placed at adjacent segments, resulted in fewer revision surgeries over a two to seven-year follow-up period, compared to patients who underwent fusion. Dr. Knaub explains, “By preserving range-of-motion, the artificial discs appear to slow or prevent the progression of disease to adjacent segments; only about 6 percent of patients who receive an artificial disc require surgery for disease at an adjacent segment. About 12 percent of patients who undergo fusion will need fusion at an adjacent segment within seven years.”
Surgical procedures for cervical disc arthroplasty tend to be significantly longer than for fusion, which should be considered for patients with significant co-morbidities. Heterotopic ossification may also be a complication.5
Mark A. Knaub, MD
Orthopaedic Spine Surgeon
Associate Director, Penn State Spine Center
Assistant Professor, Orthopaedics and Rehabilitation
Phone: 717-531-4837
Email: mknaub@pennstatehealth.psu.edu
Fellowship: Spine surgery, William Beaumont Hospital, Royal Oak, Mich.
Residency: Orthopaedic surgery, University of Pittsburgh Medical Center, Pittsburgh, Pa.
Medical School: University of Pittsburgh School of Medicine, Pittsburgh, Pa.
Connect with Mark A. Knaub, MD, on Doximity
References
- Hu Y, Lv G, Ren S, Johansen D. 2016. Mid- to long-term outcomes of cervical disc arthroplasty versus anterior cervical discectomy and fusion for treatment of symptomatic cervical disc disease: a systematic review and meta-analysis of eight prospective randomized controlled trials. PLoS One. Feb 12;11(2):e0149312.
- Zhu Y, Tian Z, Zhu B, et al. 2015. Bryan cervical disc arthroplasty versus anterior cervical discectomy and fusion for treatment of cervical disc diseases: A meta-analysis of prospective randomized controlled trials. Spine. Dec 10. [Epub ahead of print].
- Zhong ZM, Zhu SY, Zhuang JS, et al. 2016. Reoperation after cervical disc arthroplasty versus anterior cervical discectomy and fusion: a meta-analysis. Clin Orthop Relat Res. May;474(5):1307-16.
- Zhu Y, Zhang B, Liu H, et al. 2016. Cervical disc arthroplasty versus anterior cervical discectomy and fusion for incidence of symptomatic adjacent segment disease: a meta-analysis of prospective randomized controlled trials. Spine. Feb 26. [Epub ahead of print].
- Alvin MD, Abbott EE, Lubelski D, et al. 2014. Cervical arthroplasty: a critical review of the literature. Spine J. Sep 1;14(9):2231-45.

