Cartilage Grafting Options for Large or Microfracture-resistant Osteochondritis Dessican (OCD) Lesions of the Talus
Treatment options for large talar osteochondral lesions (greater than 1.5 cm) or those that fail to adequately respond to microfracture, have broadened over the last decade, with most procedures directly aimed at hyaline-like cartilage restoration. Michael Aynardi, MD, orthopaedic surgeon and assistant professor of orthopaedics, Penn State Bone and Joint Institute, says, “Patients with these types of lesions usually experience significant functional limitations and, due to lesion size, are not good candidates for microfracture and require a more invasive reconstructive approach.” Options include autologous chondrocyte implantation (ACI), osteochondral autograft transfer system (OATS), matrix-induced autologous chondrocyte implantation (MACI) and allograft cartilage grafting combined with the autologous mesenchymal stem cells (MSCs). Procedures such as OATS require a formal osteotomy to expose the lesion and gain access into the ankle joint to deliver the graft. Newer techniques such as MACI and allograft cartilage grafting can be performed without using an osteotomy and use a technique called distal tibial plafondplasty to access the joint.1
“For larger talar OCD lesions, I recommend using an allograft cartilage scaffold seeded with autogenous MSCs harvested from bone marrow aspirated from the patient’s hip. Exposure of the articular surface can be achieved through a plafondplasty of the distal tibia. With this technique, the morbidity from harvesting cartilage from the patient’s knee and the complications of the osteotomy can be avoided,” says Dr. Aynardi. Pain in the knee following harvest can be as high as 50 percent.2 In addition, an osteotomy slows recovery since the patient must wait for the bone to heal before placing weight on the limb. With tibial plafondplasty, non-perpendicular access to the talar dome is achieved using standard soft tissue exposure combined with limited anterior resection of a small, stable, triangular wedge of bone from the articular surface of the distal tibia.1 “It allows for near complete access to the joint and exposure of the articular surface without added complications and morbidity associated with other techniques,” Dr. Aynardi notes (Images A-C).
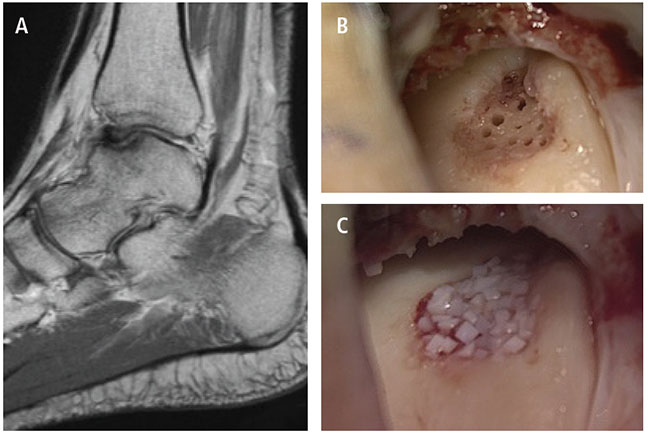
Case: 35-year-old female, recreational athlete with prior OCD of the talus. No history of trauma; had prior microfracture and scope at an outside institution. She continued to do poorly. MRI showed worsening of the lesion. Indicated for allograft cartilage grafting (DeNovo) with the addition.
(A) T1 Sagital MRI demonstrating an OCD lesion of the talus.
(B) The OCD lesion is visualized through a tibial plafondplasty. The lesion has been debrided to stable cartilage base; the subchondral bone has been stimulated.
(C) The allograft cartilage is used to fill the lesion (DeNovo). Following graft implantation, fibrin glue will be applied and mesenchymal stem cells from the patient’s bone marrow will be injected into the ankle onto the lesion.
The next steps are to insert an allograft cartilage graft and secure it with fibrin glue. Lastly, the patient’s own MSCs are injected into the ankle joint over the lesion; the MSCs will use the allograft as a scaffold and differentiate and grow into hyaline-like cartilage (Images B and C). Dr. Aynardi notes, “The MSCs form hyaline-like cartilage. This repair is durable and is desirable since it has biomechanical properties similar to the native cartilage.” As a final step, remaining bone marrow aspirate is injected into the operative site, because, as Dr. Aynardi explains, “The aspirate contains a variety of growth factors and proteins important for MSC survival and development into cartilage-forming chondrocytes.”
Treatments for large chondral defects are likely to continue to evolve, as emerging tissue bioengineering technologies are developed for clinical use, in Dr. Aynardi’s opinion. “With the increasing availability of three-dimensional printer technologies, it’s feasible that a three-dimensional scan of a patient’s cartilage defect could be used to create a bioengineered scaffold that exactly fills the defect. The scaffold could be seeded with the patient’s MSCs and other supportive proteins and growth factors,” he says. While such a treatment may seem farfetched, it brings together existing technologies, and presents a strategy for limiting secondary morbidity and yielding successful cartilage healing.
Michael C. Aynardi, MD
Orthopaedic Surgeon, Foot and Ankle
Associate Professor, Orthopaedics
Phone: 717-531-5638
Email: maynardi@pennstatehealth.psu.edu
Fellowship: Orthopaedic foot and ankle surgery, MedStar Union Memorial Hospital, Baltimore, Md.
Residency: Orthopaedic surgery, Thomas Jefferson University Hospital, Philadelphia, Pa.
Medical School: Jefferson Medical College, Philadelphia, Pa.
Connect with Michael C. Aynardi, MD, on Doximity
References:
- Peters PG, Parks BG, Schon LC. 2012. Anterior distal tibia plafondplasty for exposure of the talar dome. Foot Ankle Int. 33(3):231-5.
- Reddy S, Pedowitz DI, Parekh SG, Sennett BJ, Okereke E. The morbidity associated with osteochondral harvest from asymptomatic knees for the treatment of osteochondral lesions of the talus. Am J Sports Med. 2007;35:80-85.
