RNA Sequencing May Help Predict Severity of Ulcerative Colitis Based on Elevated Colonic Mucin Expression
Using RNA sequencing and live tissue samples from colectomy patients, researchers at Penn State Health Milton S. Hershey Medical Center and Penn State College of Medicine have found that severity of ulcerative colitis (UC) may be related to colonic mucin production.¹
No diagnostic test currently exists to determine the severity of a patient’s UC. “Finding objective criterion is very difficult, but time-to-surgery is one such indicator because the goal of UC medical treatment is to avoid surgery,” said Dr. Walter Koltun, chief, Division of Colorectal Surgery at the Milton S. Hershey Medical Center. An estimated 10 to 40% of UC patients require surgery during the course of their disease, and there is no way to predict which patients will justify the need for eventual surgery.²
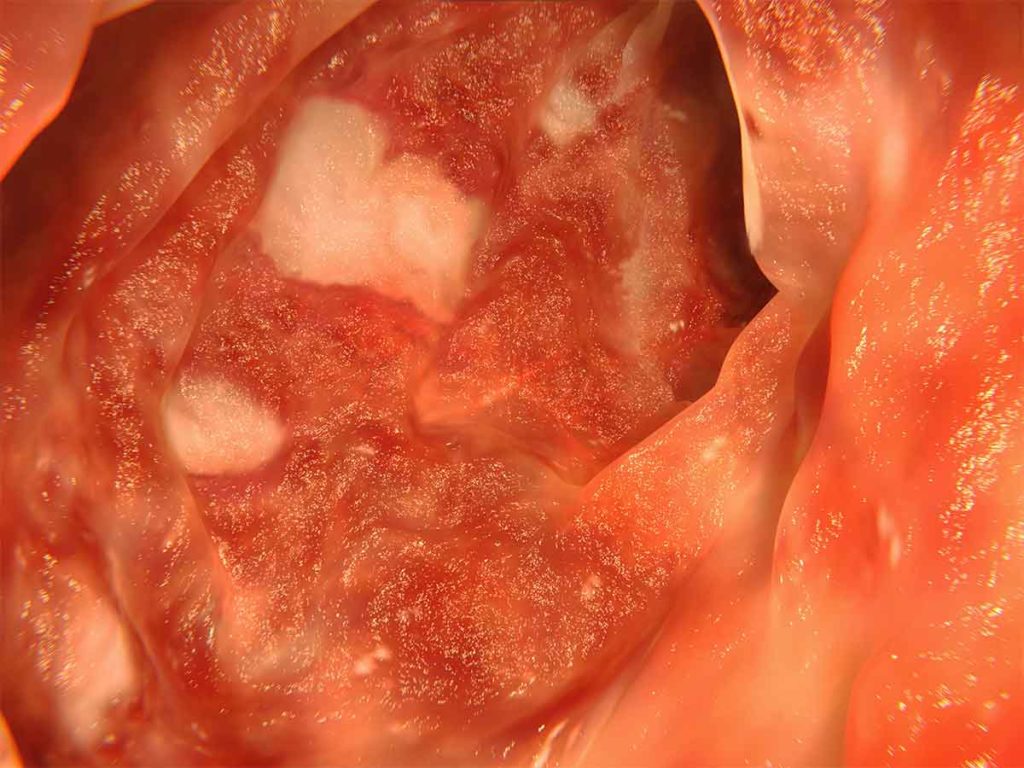
Artwork based on an endoscopic image of the colon affected by ulcerative colitis.
Both genetic and environmental factors contribute to the development and persistence of UC. “Multiple genes have been associated with UC, probably because there are multiple mechanisms for bowel injury, and which genes or pathways are most causative in any one patient is difficult to define,” Koltun said.
To try and identify which genetic pathways may play a role in causing more severe disease in UC, researchers relied on the Hershey Medical Center Colorectal Disease Biobank. It’s a unique repository which harvests both blood and tissue at the time of surgery from colorectal surgery patients for the purpose of collaborative research between clinicians and basic scientists. Now
active for 23 years, the Biobank includes samples from nearly 5,000 patients, about 1,600 to 1,700 of which have surgically resected tissue samples.
“Because we have such a large selection of samples, we’re able to control for multiple variables—such as patient age and lifestyle factors—that could give us conflicting results,” said Gregory Yochum, PhD, associate professor in the Department of Biochemistry and Molecular Biology, and associate professor in the Department of Surgery at the College of Medicine, who spearheaded the study.
During the study, researchers ran 26 full-thickness colonic tissue samples taken from UC patients undergoing colectomy for RNA sequencing. They then used a statistical evaluation to determine how similar the patients were in their expression of RNA.
They found two subsets which were distinguished by 957 differentially expressed genes. Patients in Cluster 1 were enriched in genes associated with intestinal epithelial cell differentiation. “These patients expressed higher levels of mucins, which create a gelatinous coat that protects the intestinal epithelium,” Yochum said. Patients in Cluster 2 were enriched in genes associated with epithelial-to-mesenchymal transition and inflammatory responses. They expressed lower levels of mucins.
Researchers then took patients from the two clusters and looked for differentiating factors based on their electronic medical records. The one correlation: time to surgery. Of patients with Cluster 1 genes, elevated MUC5, MUC4 and MUC2 mucin expression displayed the strongest correlation with increased time to surgery, meaning those patients potentially had a less severe form of UC.
While the research carries hope for a better way of evaluating UC severity, it also brings possible opportunities for advanced UC treatment. Typical UC treatments include the use of immunosuppression drugs like infliximab or steroids that work to reduce inflammation and manage patients’ symptoms.
“However, now that we know mucous plays a role in UC, we could someday see both immune-mediated and mucous-mediated treatments that could provide synergistic and possibly more potent patient management,” Koltun said.

Walter A. Koltun, MD
Chief, Colorectal Surgery, Penn State Health Milton S. Hershey Medical Center
Director, Carlino Family Inflammatory Bowel Disease Center
Professor of Surgery, Penn State College of Medicine
Peter and Marshia Carlino Chair in Inflammatory Bowel Disease
Phone: 717-531-5164
Email: wkoltun@pennstatehealth.psu.edu
Fellowship: Colon and rectal surgery, Lahey Hospital and Medical Center, Burlington, Mass.
Residency: General surgery, Brigham and Women’s Hospital, Boston
Medical School: Harvard Medical School, Boston
Connect with Walter A. Koltun, MD, on Doximity
Gregory Yochum, PhD
Associate Professor, Department of Biochemistry and Molecular Biology
Associate Professor, Department of Surgery, Penn State College of Medicine
Phone: 717-531-2091
Email: gsy3@psu.edu
Connect with Penn State Health Gastroenterology and Hepatology on Doximity
References
- Eshelman MA, Jeganathan NA, Schieffer KM, Kline BP, Mendenhall M, Deiling S, Harris L, Koltun WA, Yochum. Elevated colonic mucin expression correlates with extended time to surgery for ulcerative colitis patients. J Gastrointestin Liver Dis. 2019;28:405-413. Doi: https://doi.org/10.15403/jgld-250
- Windsor A, Michetti P, Bemelman W, Ghosh S. The positioning of colectomy in the treatment of ulcerative colitis in the era of biologic therapy. Inflamm Bowel Dis. 2013;19:2695-2703. Doi: :10.1097/ MIB.0b013e318292fae6

