Laparoscopic Surgery Options for IBD: When, Why, and Where?
For patients with inflammatory bowel disease (IBD), surgery is often necessary to manage symptoms and address disease-related complications. Such surgery is particularly common for patients with stricturing or fistulizing Crohn’s disease, patients with ulcerative colitis whose disease is not adequately managed with medication, and those with precancerous lesions. Surgical interventions vary according to the disease. Because Crohn’s disease can involve any segment of the gastrointestinal tract, surgical intervention is unlikely to be curative and is reserved to treat the complications of the disease such as obstruction or fistuli. As Walter Koltun, MD, explains, “Excessive or repeated resection can potentially leave a Crohn’s patient with crippling short bowel syndrome and so alternate surgical therapies are performed such as stricturplasty, which overcomes the obstruction but minimizes resection.”
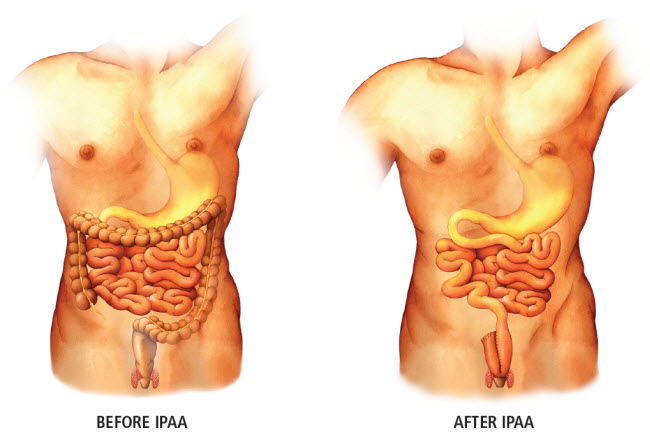
By contrast, surgery can be curative in patients with ulcerative colitis. Koltun says, “In ulcerative colitis, inflammation and disease are limited to the colon, and so complete removal of the colon eliminates the disease and represents a full cure. For ulcerative colitis patients who undergo a proctocolectomy, a subsequent reconstruction with ileal pouch anal anastomosis (IPAA) is the surgical procedure of choice.” Although technically demanding and typically only performed at specialty surgical centers, this operation presents several important advantages over the more conventional total proctocolectomy with ileostomy—the most obvious being that IPAA patients maintain bowel continence and defecate normally through the anus. During the IPAA procedure, the colon is removed and a new fecal reservoir is created using a portion of the healthy small intestine, which is anastomosed directly to the anus. Typically, a temporary ileostomy is also created, and after a two-month healing period, the ileostomy is taken down and flow of feces through the anus is re-established.
Koltun notes, “As minimally invasive surgical techniques and devices have become available, we have incorporated these into our colorectal surgery practice for IBD patients.” Currently, Penn State Health Milton S. Hershey Medical Center is among the leaders in terms of the number of laparoscopic surgeries performed on IBD patients. Unlike open surgeries, laparoscopic procedures result in a smaller incision and shorter recovery time, and are linked to fewer surgery-related infections and complications. The smaller incisions are especially important to IBD patients who are usually younger and may require repetitive surgery in the future. “We perform 200-250 major operations on IBD patients per year, and depending on degree of disease severity, about 30-40 percent of these are managed at least in part laparoscopically. Crohn’s disease is commonly treated with laparoscopic surgery that gets the patient out of the hospital usually in two to four days. For ulcerative colitis patients, we have completed more than 400 IPAA procedures, increasingly via the laparoscopic technique, and more than forty without even a temporary ileostomy. These numbers continue to increase over time as the number of patients we treat rises.”
Although approximately 5 percent of patients experience complications from IPAA surgery that result in placement of a permanent ileostomy, Medical Center IPAA patients surveyed had an average satisfaction of 9.2 (on a scale of one to 10). Koltun says, “Most of these patients resume their pre-illness level of activity and commonly state that they should have had the surgery sooner.”

Walter A. Koltun, MD
Chief, Colorectal Surgery, Penn State Health Milton S. Hershey Medical Center
Director, Carlino Family Inflammatory Bowel Disease Center
Professor of Surgery, Penn State College of Medicine
Peter and Marshia Carlino Chair in Inflammatory Bowel Disease
Phone: 717-531-5164
Email: wkoltun@pennstatehealth.psu.edu
Fellowship: Colon and rectal surgery, Lahey Hospital and Medical Center, Burlington, Mass.
Residency: General surgery, Brigham and Women’s Hospital, Boston
Medical School: Harvard Medical School, Boston
Connect with Walter A. Koltun, MD, on Doximity

