Researchers evaluate COVID-19’s impact on IBD patients, GI fellowship training in two separate studies
COVID-19 brought with it numerous questions and concerns for people with gastroenterological conditions and the providers who care for them. Clinical researchers at Penn State Health Milton S. Hershey Medical Center were involved in two multi-institutional collaborative studies, one to evaluate the impact of coronavirus disease on clinical course of inflammatory bowel disease (IBD) including treatment, and the other to determine the impact of COVID-19 on gastroenterology (GI) and hepatology fellows’ training in the United States.
Risk for severe COVID-19 in IBD patients
As part of their treatment regimen for IBD, patients often use medications including biologics, small molecules and steroids that suppress the immune system. While a worldwide registry—Surveillance Epidemiology of Coronavirus Under Research Exclusion—has reported the clinical course of COVID-19 among IBD patients and the factors associated with severe COVID-19. there is still an evolving understanding and limited data comparing the clinical characteristics and outcomes among IBD patients with COVID-19 compared to patients without IBD in the U.S.
“So, we put together a multi-institutional group of people to review large data sets to help give us a better understanding about the relationship between COVID-19 and IBD,” said Dr. Kofi Clarke, chief of the Division of Gastroenterology and Hepatology at the Milton S. Hershey Medical Center.
Using a federated health research network data set (TriNetX), the collaborators performed a search and analysis of electronic health records and identified 232 IBD patients diagnosed with COVID-19 in the U.S. between Jan. 20 and May 26, 2020. They then compared various clinical data points in their electronic health records with those of non-IBD patients diagnosed with COVID-19 during the same period.
In an unadjusted analysis, there was no difference in the risk of severe COVID-19 between the IBD and non-IBD patients. After propensity score matching, both groups were well-balanced with a similar risk of severe COVID-19.¹ “These results gave us an added level of evidence showing that IBD patients are not at a significantly increased risk for severe COVID-19 despite immunosuppressive treatment,” Clarke said.
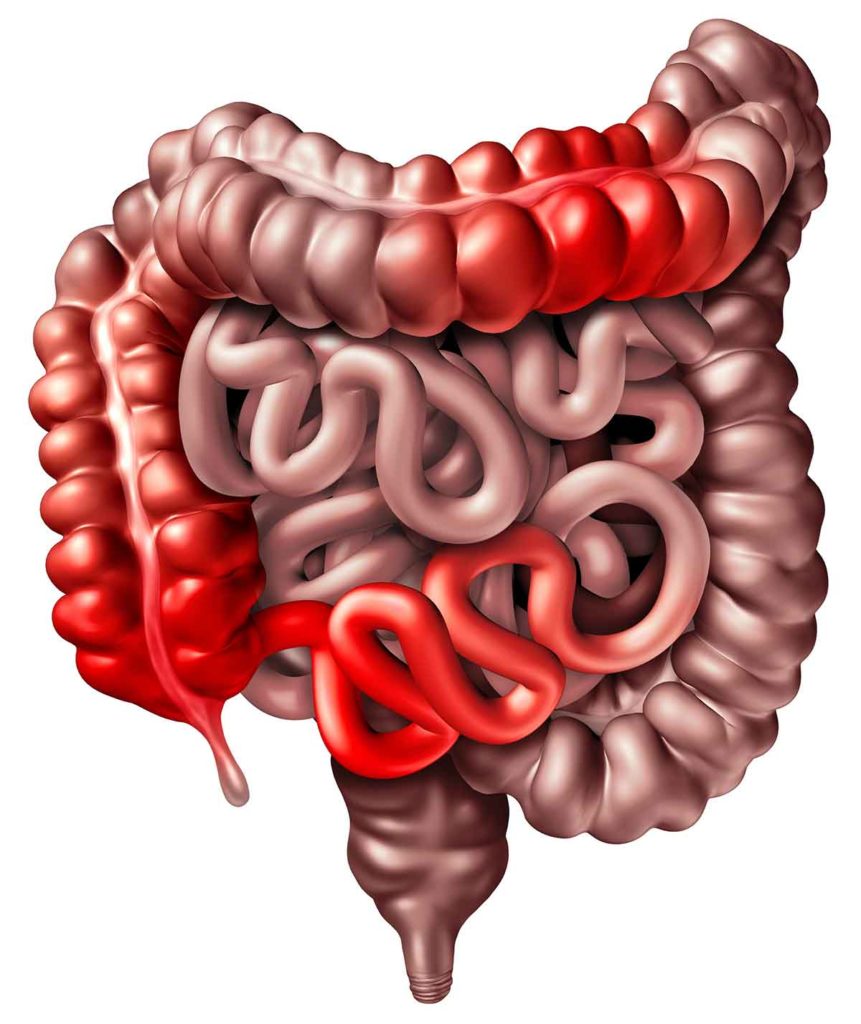
Illustration of inflammation due to inflammatory bowel disease causing obstruction inside the intestinal tract.
Because the results showed no increased risk, providers should encourage IBD patients to remain on immunosuppressant therapy during the pandemic. Patients who test positive for COVID-19 need to be evaluated by a clinical provider for COVID-19 symptoms, date since dose of last treatment and severity and activity of underlying IBD. With that complete data, providers can then provide recommendations on their medication dosing.
Clarke’s research collaborators included Shailendra Singh, Ahmad Khan and Monica Chowdhry with West Virginia University Health Sciences Division; Mohammad Bilal with Beth Israel Deaconess Medical Center; and Gursimran S. Kochhar with Allegheny Health Network.
Assessing COVID-19’s impact on U.S. GI and hepatology fellows
During COVID-19’s first wave U.S. wave in March 2020, professional societies asked hospitals to cancel and reschedule elective procedures and endoscopies. That stoppage also impacted the education for GI and hepatology fellows in the U.S., a significant number of whom were graduating in June 2020.
To learn more about fellows’ perceptions, changes in clinical duties and education during the pandemic, researchers distributed a questionnaire nationwide. A total of 177 GI fellows responded. The results showed that COVID-19 impacted all aspects of U.S. GI fellowship training—endoscopy, outpatient clinics, inpatient consults and educational activities. Specifically:
- 29.4% of fellows were redeployed to non-GI services during the pandemic.
- 72.4% reported some type of restriction on endoscopic participation, but only about one-third believed such restriction was warranted, and the majority were concerned about the pandemic’s impact on endoscopic competency.
- 72.5% reported their programs provided increased wellness resources.
- 17.6% of respondents with children reported no support with child care.²
The results reflected GI trainees concerns about having enough skills to feel confident on graduation, their need for more resources to handle COVID-19-related stressors, and a desire to be consulted prior to their professional groups making major decisions such as surgery stoppages.
“One of the biggest takeaways is the importance of faculty members asking fellows, ‘How are you feeling and how can we support you?’” Clarke said. “We must recognize fellows are also people with real-life concerns.”
Clarke’s research collaborators included Bilal; Sergio A. Sanchez-Luna from Allegheny Health Network; Shannon Dalessio and Jennifer L. Maranki with Penn State College of Medicine; and Shazia Mehmood Siddique with the University of Pennsylvania Perelman School of Medicine.

Kofi Clarke, MD, FACP, FRCP, AGAF
Division Chief, Gastroenterology and Hepatology, Penn State Health Milton S. Hershey Medical Center
Phone: 717-531-4950
Email: kclarke@pennstatehealth.psu.edu
Fellowship: Gastroenterology and hepatology, University of Pittsburgh Medical Center, Pittsburgh, Pa.; Research Fellowship: Michigan State University, East Lansing, Mich.
Residency: Internal medicine, Temple University School of Medicine, Western Pennsylvania Hospital, Pittsburgh, Pa.; Gastroenterology and hepatology, Royal College of Physicians, London
Medical School: University of Ghana Medical School, Ghana
Postgraduate: Medicine, Gastroenterology and hepatology, Imperial College, London
Connect with Kofi Clarke, MD, FACP, FRCP, AGAF, on Doximity
References
- Singh S, Khan A, Chowdhry M, Bilal M, Kochhar G, Clarke K. Risk of severe coronavirus disease 2019 in patients with inflammatory bowel disease in the United States: A multicenter research network study. Gastroenterology 2020;159:1575-1578. doi: 10.1053/j.gastro.2020.06.003
- Clarke K, Bilal M, Sanchez-Luna S.A. et al. Impact of COVID-19 pandemic on training: Global perceptions of gastroenterology and hepatology fellows in the USA. Dig Dis Sci. 2020 Oct 19;1-5. doi: https://doi.org/10.1007/s10620-020-06655-y

