When Skipping a Step is a Good Thing: Stoma-Free Ileal Pouches for Ulcerative Colitis
Physicians at Penn State Health Milton S. Hershey Medical Center have long offered patients an alternative to the three-step ileal pouch anal anastomosis (IPAA) or ileal pouch procedure. The operation creates an internal pouch to allow fairly normal defecation, without a stoma, for individuals with ulcerative colitis or familial adenomatous polyposis. Rather than require all patients to proceed through the three traditional stages of colon removal, internal pouch and loop ileostomy, and ileostomy closure for the operation, the Milton S. Hershey Medical Center surgeons offer healthy patients two or fewer steps.
“Most people never get an ileal pouch without a stoma,” says Walter Koltun, MD, chief of the Division of Colon and Rectal Surgery at Hershey Medical Center and director of the Penn State Inflammatory Bowel Disease (IBD) Center. “But here, we have two unique approaches to make that not just possible, but a regular occurrence.”
First, if a patient is healthy at the initial consult, Dr. Koltun or one of his fellow surgeons will do a one-stage procedure to remove the colon and connect the pouch with no stoma. The second circumstance, which is increasingly common at the IBD Center, is to start the procedure as if it will be a three-stage operation. During the six-month waiting period between stages, some patients become much healthier, and surgeons are able to skip the middle stage to go straight to the final stage, without the interim loop ileostomy.
These options come in addition to the group’s standard two-stage procedure offered to patients who are healthy enough to start with colon removal, internal reservoir and temporary loop ileostomy, followed by a closure of the ileostomy two months later. In total, Dr. Koltun says the team performs four to six stoma-free IPAA operations per year—about 17 percent of their IPAA caseload.
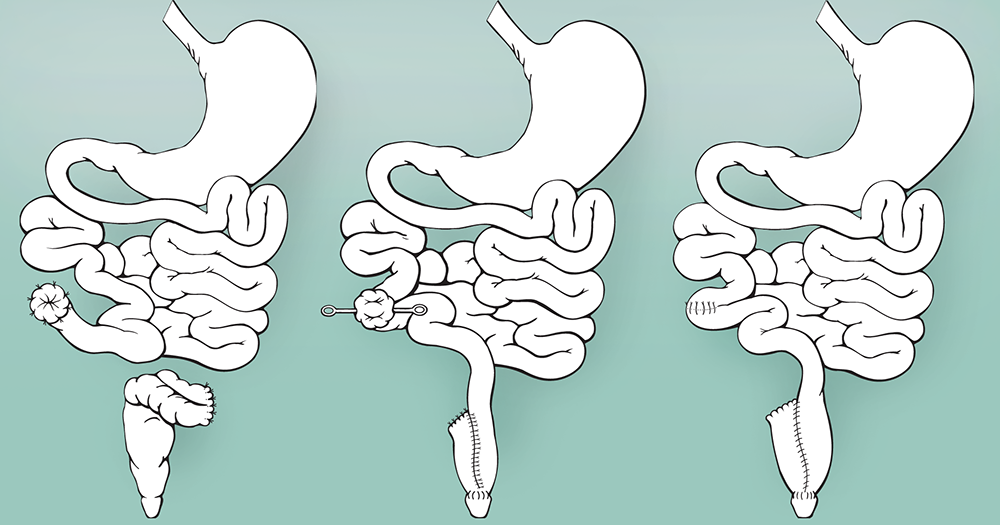
Figure 1. The traditional IPAA procedure has three stages. First, the colon is removed. Six months later, an internal reservoir and a temporary loop ileostomy are created. Two months later, the ileostomy is closed. At the Penn State IBD Center, patients with significant improvement in health following the first stage of a planned three-stage procedure can now proceed directly to the final step, skipping the intermediary operation.
“We’re approaching our 100th stoma-free procedure, out of the 600 or more our team has performed in the past 20 years,” says Dr. Koltun. “For young and otherwise healthy people, IPAA is the procedure of choice. If they’re off immunosuppressants and well nourished at the start or after the first stage, why bother with a stoma?”
Dr. Koltun and his colleagues are also well versed in managing this complex surgery under complicated medical circumstances, including patients taking biological drugs, patients who have had colon removal and stoma operations done at other institutions, and patients who have cancer and require chemotherapy in between IPAA stages.
“In the appropriately selected patient, we can often do the IPAA in fewer steps, without a stoma,” says Dr. Koltun. “But even for patients who have circumstances that complicate surgical management, we’re used to those challenges, and we take care of them on a regular basis, allowing them to return to gastrointestinal continuity as soon as possible.”
In addition to their surgical expertise, the IBD team at Hershey Medical Center regularly publishes on IPAA-related topics, such as pouchitis—inflammation of the ileal pouch that, when chronic or serious, can require removal of the ileal pouch and placement of a permanent stoma. Dr. Koltun and his team’s identification of genetic variants that may predispose to pouchitis via imbalance of gut bacteria, published recently in the Journal of Crohn’s and Colitis, could form the basis of future research into identifying which patients are most likely to have post-operative complications.1
“We are trying to define genetic determinants of surgical outcomes. Some people do better with the pouch than others, and if we can determine who will do well and who won’t, then this can assist with surgical decision-making,” Dr. Koltun says. “The bottom line is that doing this surgery is very tricky, and there are a lot of details that make a difference to performance and successful outcomes. We have a great deal of experience, but if there’s any other way to improve our ability to help patients who need this surgery, we want to find it.”
The group’s work further extends into the field of inflammatory bowel diseases, courtesy of an assertive research program. Another recent ulcerative colitis study of the team’s appeared last year in PLoS One, revealing an association between reduced total serum bilirubin levels and ulcerative colitis diagnosis.2
The research program benefits from the fact that every patient undergoing IPAA—or any other operation—at the medical center’s IBD Center is approached to donate blood, serum and tissue to their biobank at the time of surgery. As a result, the biobank contains samples from more than 3,500 patients (growing by about 400 per year), enabling the team to make progress on their nearly two dozen current studies on genetic and other determinants of disease and surgical outcomes.
References:
- Schieffer KM, Wright JR, Harris LR, Deiling S, Yang Z, Lamendella R, Yochum GS, Koltun WA. NOD2 Genetic variants predispose one of two familial adenomatous polyposis siblings to pouchitis through microbiome dysbiosis. J Crohns Colitis. 2017 Oct 27;11(11):1393-1397.
- Schieffer KM, Bruffy SM, Rauscher R, Koltun WA, Yochum GS, Gallagher CJ. Reduced total serum bilirubin levels are associated with ulcerative colitis. PLoS One. 2017 Jun 8;12(6):e0179267.

Walter A. Koltun, MD
Chief, Colorectal Surgery, Penn State Health Milton S. Hershey Medical Center
Director, Carlino Family Inflammatory Bowel Disease Center
Professor of Surgery, Penn State College of Medicine
Peter and Marshia Carlino Chair in Inflammatory Bowel Disease
Phone: 717-531-5164
Email: wkoltun@pennstatehealth.psu.edu
Fellowship: Colon and rectal surgery, Lahey Hospital and Medical Center, Burlington, Mass.
Residency: General surgery, Brigham and Women’s Hospital, Boston
Medical School: Harvard Medical School, Boston
Connect with Walter A. Koltun, MD, on Doximity

