The Posteromedial Tibial Plateau Fracture: New Perspectives
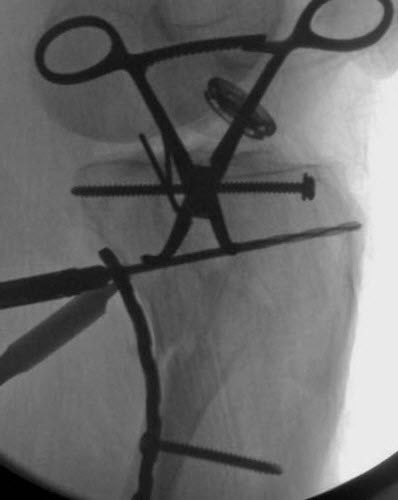
Fractures of the posteromedial tibial plateau are challenging to treat, owing to their complexity and unfamiliar surgical approach. J. Spence Reid, MD, Penn State Bone and Joint Institute explains, “This fracture pattern may occur as part of a fracture-dislocation in which it is often associated with an ACL tear, or as part of a bicondylar tibial plateau fracture.” The typical fracture pattern is shown here, visualized with both a standard radiograph, and a three-dimensional computed tomography (CT) scan, (figures A and B) from one of Reid’s cases.
The fracture pattern is usually quite vertical and unstable, with a high shearing angle, and encompasses a large proportion (greater than 25 percent) of the plateau area, with a fragment that is displaced by more than five millimeters. There is often posterior subluxation of the femoral condyle which can have a rotatory component in a fracture–dislocation pattern. Minimally displaced fractures can be treated non-operatively, but these are rare. Displaced fractures should be surgically stabilized to restore joint congruity and prevent late subluxation. In the case of a displaced bicondylar fracture, a staged treatment technique is often employed in which a simple spanning external fixator is placed at the time of injury, and surgical reconstruction is delayed until the soft tissues have recovered, usually between seven and fourteen days. When an ACL injury is also present, reduction and fixation of the posteromedial plateau helps protect the ACL repair or reconstruction by preventing rotatory subluxation of the femoral condyle. Moreover, Reid notes, “Several recent anatomic and biomechanical studies have shown that a locked plate placed from the lateral side of the proximal tibia does not capture and stabilize a typical posteromedial fragment. A direct posteromedial approach and antiglide plate are usually needed.”
Reid typically uses a modified Lobenhoffer approach to gain access to the posteromedial plateau. Often this is done with the patient in the supine position as part of a combined medial and lateral reconstruction for a bicondylar fracture. The skin incision is made along the medial head of the gastrocnemius muscle extending from the medial femoral epicondyle proximally to the posterior border of the tibia six to eight centimeters beyond the tip of the posteromedial fragment distally. The deep interval is between the gastrocnemius muscle which is retracted posteriorly and the pes anserinus, which is retracted anteriorly. In this approach, the articular surface can be visualized via a submeniscal arthrotomy if needed. When the fragment is large, and non-comminuted, the reduction can be achieved at the level of the metaphysis and verified at the joint line via fluoroscopy or by direct observation. The reduction maneuver is traction on the tibia and extension of the knee. Anterior translation of the femur is often needed. A medially placed femoral distractor may be useful to regain length. Reduction can be maintained with a Kirchner wire and a pointed reduction clamp. An antiglide buttress plate consisting of a small fragment third tubular or reconstruction plate is sufficient. There are also newer, site-specific pre-contoured plates available. Reid notes, “The key is to place the first screw just distal to the apex of the fragment on the intact tibial cortex,” the slightly under-contoured plate aids reduction as the screw is tightened (figure C).
In the case of a very large fragment, an anterior to posterior lag screw just under the articular surface may be added.
J. Spence Reid, MD
Orthopaedic Surgeon, Trauma
Professor, Orthopaedics and Rehabilitation
Phone: 717-531-1363
Email: jreid@pennstatehealth.psu.edu
Fellowship: Orthopaedic trauma, R. Adams Cowley Shock Trauma Center, Baltimore, Maryland
Residency: Orthopaedic surgery, Penn State Health Milton S. Hershey Medical Center, Hershey, Pa.
Medical School: Penn State College of Medicine, Hershey, Pa.
Connect with Penn State Bone and Joint Institute on Doximity