Measurement of Tibial Tubercle to Trochlear Groove (TT-TG) Distance by MRI for Patellofemoral Instability
Patellar instability, with repeated lateral dislocation, commonly seen in younger, active adults, is associated with a number of anatomical pathologies and usually requires surgical intervention. Among these, increased tibial tubercle to trochlear groove (TT-TG) distance is a prominent risk factor. TT-TG distance describes the degree of lateralization of the tibial tubercle. “TT-TG distance is routinely measured in most patients who present with a partial or complete knee-cap dislocation. This makes it an accessible piece of information that could potentially be used to identify patients at-risk for repeated dislocations,” explains Paul Sherbondy, MD, Penn State Bone and Joint Institute.
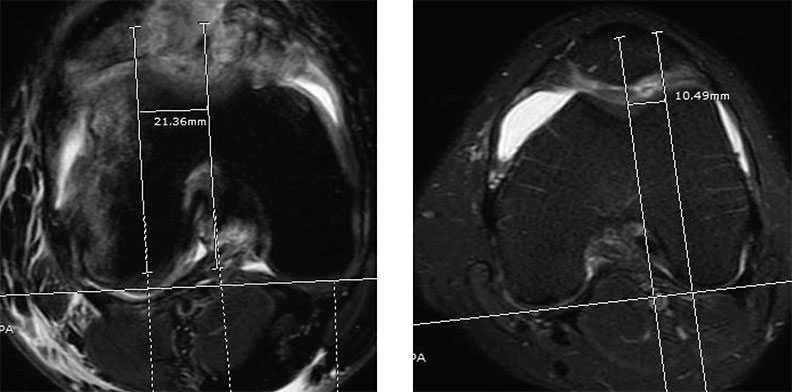
Analysis of MRIs reveals increased TT-TG distance of 21.36 mm in a patient with repeated patellar dislocation (left), compared to TT-TG distance of 10.49 mm in a patient without patellar dislocation (right).
Using MRI in a recent series of cases, Dr. Sherbondy and Ashley Anderson, MD, Penn State sports medicine orthopaedics fellow, found average TT-TG distances of 12-13 mm in patients with repeated patellar dislocation (n=30), compared to 9-10 mm in normal controls without dislocation (n=38) (Figure). These TT-TG distances are smaller than previously described using CT scan. In one early study using CT scans, Dejour, et al.,1 found that average TT-TG distance in repeated dislocators was greater than or equal to 20 mm, compared with 12-13 mm in controls. MRI measures, however, are known to be consistently smaller than those obtained with CT.2 Therefore, the threshold defined by Dejour cannot be applied to patients for whom MRI was performed.
Dr. Sherbondy explains, “MRI measurements in our study showed high inter-rater reliability and little variation between patients,” indicating these values are highly reproducible and accurate. To determine TT-TG distance, Dr. Sherbondy notes, “MRI might be preferred since it’s widely used, does not expose the patient to radiation, and provides information about related injuries and pathology, like damage to the medial retinaculum and articular cartilage, bone bruising or presence of loose bodies from trauma.”
No clear thresholds currently exist for defining TT-TG distances, using MRI, that predict repeated patellar dislocation. Dr. Sherbondy notes, “There are no large epidemiological studies that definitively characterize TT-TG distance in the general population and in clinical populations like patients with repeated patellar dislocation.”
The new findings from Drs. Sherbondy and Anderson add to the understanding about normal versus abnormal TT-TG distance. Future, larger-scale investigations using MRI that clearly define a threshold for what constitutes an abnormally large TT-TG distance could help guide clinical decisions regarding whether and what type of surgical intervention is most appropriate for patients with patellar dislocation. Dr. Sherbondy adds, “With a high TT-TG distance, it might be helpful to perform a tibial tubercle osteotomy. With other types of pathology, a medial patellofemoral ligament reconstruction (MPFL) may be adequate to address the problem.”

Paul Sherbondy, MD
Associate Professor, Orthopaedics and Rehabilitation
Orthopaedic Sports Medicine Surgeon
Phone: 814-865-3566
Email: psherbondy@pennstatehealth.psu.edu
Fellowship: Orthopaedic Sports Medicine, Johns Hopkins University Hospital, Baltimore, Md.
Residency: Orthopaedic Surgery, Tulane University, New Orleans, La.
Medical School: Temple University School of Medicine, Philadelphia, Pa.
Connect with Paul Sherbondy, MD, on Doximity
References
- Dejour H, Walch G, Nove-Josserand L, Guier C. 1994. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 2(1): 19-26.
- Camp CL, Stuart MJ, Krych AJ, Levy BA, Bond JR, Collins MS, Dahm DL. 2013. CT and MRI measurements of tibial tubercle-trochlear groove distances are not equivalent in patients with patellar instability. Am J Sports Med. 41(8):1835- 40.
