Penn State Health is first in the region to employ the da Vinci SP to offer improved outcomes on patients with head and neck cancers
Since Intuitive Surgical gained FDA approval for use of its da Vinci platform in transoral robotic surgery (TORS) applications,1 treatment of head and neck cancers has become increasingly precise and less invasive. Now, with the advent of the company’s latest da Vinci SP system, surgeons are performing TORS to treat a wider range of otolaryngological cancers with even greater precision and fewer complications.
“With previous iterations of the robot, we were taking a square peg and trying to put it through a round hole,” said Dr. Neerav Goyal, chief of the Division of Head and Neck Oncology and Surgery, head and neck surgical oncology disease team leader and vice chair for patient safety and quality in the Department of Otolaryngology ─ Head and Neck Surgery at Penn State Health Milton S. Hershey Medical Center. “We were using robotic instruments that were initially developed for abdominal surgery and adapting them for transoral surgery, whereas with this version, [Intuitive Surgical] truly had transoral surgery in mind in its development and execution,” said Goyal, also an associate professor at Penn State College of Medicine.
The coaxial approach
With previous generations of the robot, several arms approached the patient from different angles. The SP model also makes use of multiple robotic arms; however, the arms stem from a single port to provide superior articulation. Surgeons now have an easier time fitting the instruments into the patient’s throat, which is significant when operating in constricted areas.
Over the years, five surgical oncologists at Hershey Medical Center, along with nurses and support staff, have gained extensive TORS experience with other da Vinci technologies. Goyal says the updated robot will allow the team to continue providing excellent TORS outcomes, while targeting a wider variety of tumors. Currently, surgeons are using the da Vinci SP to remove carcinomas of the tonsil, tongue and larynx, and noncancerous tumors.
“If we go back 10 or 15 years, before TORS, the primary treatment options for cancer of the tonsil and base of tongue were radiation and chemotherapy, which involve substantial time commitments and have other significant disadvantages,” Goyal said. “One of the big advantages of using the robotic tool is that it permits us to perform surgery that we could not previously perform. And in some cases, particularly cancers detected in their earlier stages, TORS may be the only modality required.”
Research indicates use of TORS in patients with early-stage oropharyngeal cancer leads to enhanced immediate outcomes and improved survival compared to patients who had nonrobotic surgery.2 And compared to the older robot, the SP model is considered a safe and effective way to perform transoral robotic surgery.3
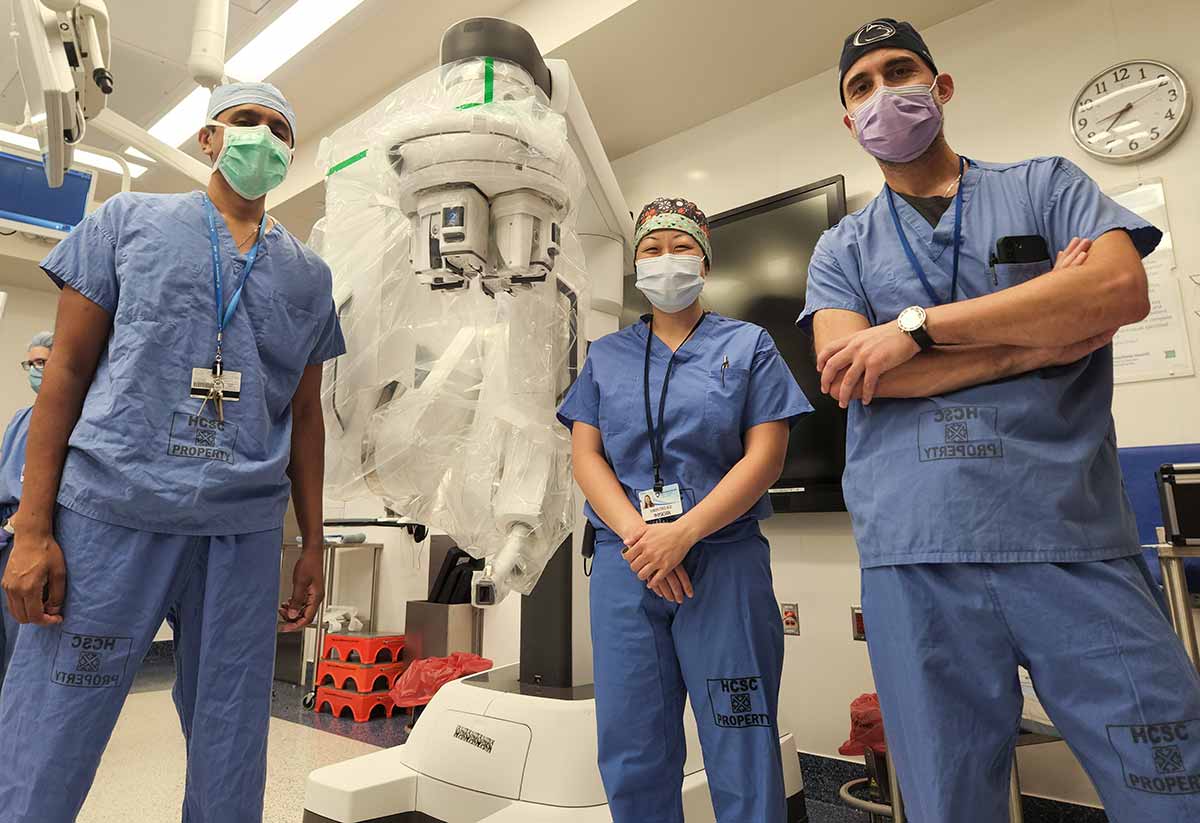
Penn State Health otolaryngologist ─ head and neck surgeons, from left, Dr. Neerav Goyal, Dr. Karen Choi and Dr. Guy Slonimsky show the da Vinci SP robotic surgical system, which they use to treat head and neck cancer. The minimally invasive platform allows for surgeons to make incisions through the mouth, which reduces pain, shortens recovery time and improves aesthetic outcomes. Not pictured: Dr. David Goldenberg and Dr. Craig Bollig.
Additional benefits
Goyal says the da Vinci SP also allows surgeons to target patients whose anatomies previously rendered minimal invasion impossible. In particular, patients with smaller mouths posed a challenge with previous robotic systems, often resulting in open surgical approaches that could include splitting the jaw or creating a much larger exposure, which are associated with comorbidities.
“Ultimately, any patient who has a head and neck cancer of the tonsil, tongue or the larynx is a possible candidate,” Goyal said. “We would have to evaluate the individual patient and the cancer to see if the cancer is accessible or if the tumor would be appropriately approachable with the robot.”
In general, patients with more advanced T3 or T4 cancers were often less likely to qualify for a robotic approach. However, in certain situations, TORS may now be appropriate because of the increased capabilities of the SP model. Goyal suggests that referring physicians allow experienced TORS providers — not previous surgical limitations or outdated best practices — to guide their treatment recommendations.
Goyal hopes to eventually be able to perform 60% to 70% of tonsil and tongue cancer surgery cases with the SP, which he says is a solid step forward for patients. “It’s the next logical evolution of the product,” he said.
Looking to the future
Tongue-base reduction surgery and sleep apnea intervention are other conditions Goyal thinks might be treated with the SP in the near future. Penn State Health researchers are also investigating the benefits of using robotic-assisted surgery for total laryngectomy, a procedure rarely performed in the United States with robotic assistance. In addition, the SP has been successfully used at Hershey Medical Center for certain urological conditions, and other specialties, such as colorectal surgery, may soon benefit as well.
“The biggest question we face in head and neck cancer is figuring out which patient will benefit from which treatment the most,” Goyal said. “Individualized medicine gets talked about a lot, but in cancer, that’s where the most value lies. If we can see why a specific tumor is a worse actor than others, we can adjust treatment. This way, we give appropriate treatment to each patient, which sometimes means less treatment, while still getting optimal results.”

Neerav Goyal, MD, MPH, FACS
Chief, Division of Head and Neck Oncology and Surgery
Associate professor and vice chair for quality and safety, Department of Otolaryngology ─ Head and Neck Surgery
Associate professor, neurosurgery and public health sciences, Penn State College of Medicine
Phone: 717-531-6822
Email: ngoyal1@pennstatehealth.psu.edu
Fellowship: Surgical oncology, head and neck, Massachusetts Eye and Ear Infirmary, Harvard Medical School, Boston
Residency: Otolaryngology, and Otolaryngology – Head and Neck Surgery, Penn State Health Milton S. Hershey Medical Center
Medical School: Jefferson Medical College of Thomas Jefferson University, Philadelphia
Connect with Neerav Goyal, MD, MPH, FACS, on Doximity
References
- Bekeny J.R., Ozer E. Transoral robotic surgery frontiers. World Journal of Otorhinolaryngology – Head and Neck Surgery. 2016 June;Vol2Iss2:130-135 (https://onlinelibrary.wiley.com/doi/10.1016/j.wjorl.2016.05.001)
- Nguyen A, Luu M, Mallen-St Clair J, Mita AC, Scher KS, Lu DJ, Shiao SL, Ho AS, Zumsteg ZS. Comparison of Survival After Transoral Robotic Surgery vs Nonrobotic Surgery in Patients With Early-Stage Oropharyngeal Squamous Cell Carcinoma. JAMA Oncology. 2020 August;6(10):1555-1562 (https://jamanetwork.com/journals/jamaoncology/fullarticle/2769670)
- Holsinger FC, Magnuson JS, Weinstein GS, Chan JYK, Starmer HM, Tsang RKY, Wong EWY, Rassekh CH, Bedi N, Hong SSY, Orosco R, O’Malley BW, Moore EJ. A Next-Generation Single-Port Robotic Surgical System for Transoral Robotic Surgery: Results From Prospective Nonrandomized Clinical Trials. JAMA Otolaryngology – Head & Neck Surgery. 2019 September;145(11):1027-1034 (https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/2749803)

