Novel Techniques for Removal of Embedded Inferior Vena Cava (IVC) Filters Reduce Risk of Long-Term Complications
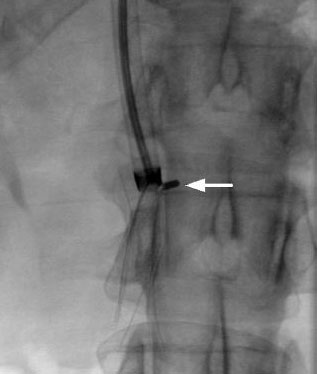
With the loop snare forcefully closed around the filter legs, the metal guide is pulled back with the filter into the sheath. The captured filter legs fold in half and the filter apex begins to invert (arrow).
Retrievable IVC filters are used to treat patients temporarily for pulmonary embolism (PE) prophylaxis, including those facing prolonged bedrest following lower-limb surgery. The devices may be removed to prevent the risk of long-term complications once there is no immediate risk of thromboembolism, with medical management superseding cardiovascular interventions.¹ Complications can include filter fracture, embolization, caval penetration, and, ironically, an increased incidence of recurrent deep vein thrombosis after filter placement.¹ Regular patient follow-up is critical for optimal outcomes, along with periodic chart reviews and multiple attempts to contact patients.¹ Inferior vena cava filters, particularly those in place for many months or years, can embed themselves in surrounding tissue, but novel techniques can often succeed in even the most complicated IVC filter removal cases.
Frank Lynch, MD, clinical professor of radiology, surgery, and medicine at Penn State Health Milton S. Hershey Medical Center, has performed more than 1,500 filter retrieval procedures. Most IVC filter removals require capture of the filter apex. When the filter is severely tilted and the apex is in contact with the caval wall and covered by an endothelial cap, a significant technical challenge exists.² One novel technique is a standard angioplasty balloon to free the apex of severely tilted filters with endothelial apical caps.² A more common, yet still complex, procedure is a modified loop snare technique in which an angled surgical wire and gooseneck snare form an in situ snare.³ The filter is withdrawn into the sheath folded over, and the filter apex inverted and pulled free from the caval wall.³
These techniques were developed in response to the rapid increase of retrievable IVC filters. “In 1999 when retrievable filters were approved in the United States, their use exploded,” says Lynch. “For example, in 2012, more than 250,000 devices were placed, up from 10,000 just a few years before. However, national retrieval rates remained low, just 15 to 20 percent.” In 2010, the FDA issued a statement strongly urging improved follow-up with these patients, many of whom began to suffer long-term complications, a position they reiterated in 2012. The FDA also challenged device manufacturers to provide additional long-term clinical data to justify the use of their retrievable IVC filters. In the future, Lynch hopes these data and advanced techniques will dispel the prevailing belief that IVC filters cannot be safely removed.

Frank C. Lynch, MD
Clinical Professor, Radiology, Surgery, and Medicine
Phone: 717-531-5418
Email: fcl3@psu.edu
Fellowship: Cardiovascular and interventional radiology, Johns Hopkins University Hospital, Baltimore, Maryland
Residency: Radiology, diagnostic, Johns Hopkins University Hospital, Baltimore, Maryland
Medical School: Penn State College of Medicine, Hershey, Pennsylvania
Connect with Frank C. Lynch, MD, on Doximity
References
- Lynch FC. A Method for Following Patients with Retrievable Inferior Vena Cava Filters: Results and Lessons Learned from the First 1,100 Patients. J Vasc Interv Radiol 2011;22:1507–1512.
- Lynch FC. Balloon-assisted Removal of Tilted Inferior Vena Cava Filters with Embedded Tips. J Vasc Interv Radiol 2009; 20:1210–1214.
- Lynch FC. Modified Loop Snare Technique for the Removal of Bard Recovery, G2, G2 Express, and Eclipse Inferior Vena Cava Filters. J Vasc Interv Radiol 2012; 23:687–690.
