Saving the Brain: Proper Anticoagulation Therapy for Patients with Atrial Fibrillation
As the population ages, increasing numbers of patients are presenting with atrial fibrillation, with the number projected to grow to more than 7.5 million in the U.S. by 2050.1 A strong correlation exists between atrial fibrillation and severe acute ischemic stroke.2 Citing large databases such as the PINNACLE-AF registry,3 Gerald Naccarelli MD, Bernard Trabin Chair in Cardiology and chief, cardiology, Penn State Heart and Vascular Institute, says, “We have known since the late 1980s that warfarin was able to reduce the risk of stroke by two-thirds in high-risk patients with atrial fibrillation. However, close to half the patients who should be on anticoagulant therapy, according to guidelines, are not receiving it.” He cites multiple co-morbidities, shifting recommendations, and bleeding risk as possible causes, but emphasizes that maintaining brain function must be a key factor in treatment planning for even the most medically complex patients.
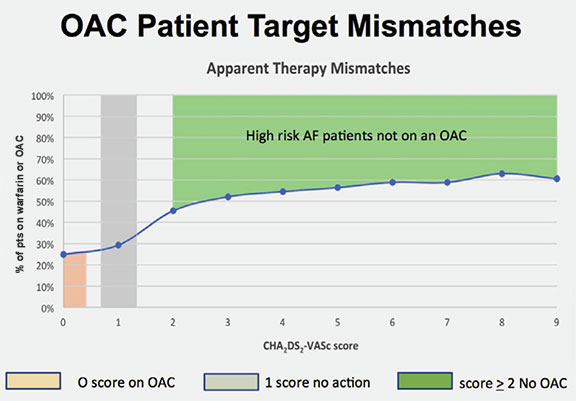
Number of eligible patients not taking oral anticoagulation (OAC). Image courtesy of Gerald Naccarelli, M.D.
Penn State Heart and Vascular Institute is piloting a study that uses data from more than 9,000 atrial fibrillation patients’ electronic medical record (EMR). With this data, they identified 43 percent of these patients with elevated CHA²DS²VASc scores greater than 2 and who were not on anticoagulation therapy to prevent strokes or systemic embolic events. The physicians are then alerted to this potential therapeutic gap or ‘mismatch’ between treatment and condition prior to each appointment, and can make a case-by-case determination on whether or not to initiate anticoagulation. Whenever a patient is admitted to Hershey Medical Center, regardless of the reason, medication reconciliation in the EMR would automatically “flag” this discrepancy between stroke risk and anticoagulation therapy, and prompt further conversation.
Frequently, it is not clear that these patients should be on anticoagulant therapy, even when suggested by the guidelines. Some patients have multiple co-morbidities, which may contraindicate the use of anticoagulants, and comparative risks are discussed under the shared decision-making system in which patients collaborate on their care. Penn State Hershey is developing tools to help clinicians stratify these risks, as well as charts to provide visuals for patients. “All the newer anticoagulants reduce the rate of even the most severe bleeding events, intracranial hemorrhage, by 50 percent,” Dr. Naccarelli states.
Dr. Naccarelli hopes that the pilot EMR alert system reduces the rate of anticoagulant “mismatches” from 45 percent to 30 percent. Given the numbers of stroke and atrial fibrillation patients, the potential impact of this program is huge. He summarizes with a mantra he often hears from neurosurgeons: “You can always transfuse blood, but you can’t transfuse brain.”

Gerald V. Naccarelli, MD
Bernard Trabin Chair in Cardiology
Professor, Medicine
Chief, Division of Cardiology
Phone: 717-531-3907
Email: gnaccarelli@pennstatehealth.psu.edu
Fellowship: Cardiology, Indiana University Medical Center, Indianapolis, Ind., and Medicine, Penn State Health Milton S. Hershey Medical Center, Hershey, Pa.
Residency: Medicine, North Carolina Baptist Hospital, Winston Salem, N.C.
Medical School: Penn State College of Medicine, Hershey, Pa.
Connect with Gerald V. Naccarelli, MD, on Doximity
References:
- Naccarelli GV, Varker H, Lin J, Schulman KL. Increasing prevalence of atrial fibrillation and flutter in the United States. Am J Cardiol. 2009 Dec 1;104(11):1534-9.
- Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. August, 1991; 22(8):983-8.
- http://www.medscape.com/viewarticle/769311. Accessed September 18, 2015.
