Penn State Health Surgeon Tests Feasibility of 4K-3D Video Microscope for Upper Airway Stimulation Surgery
Since 2019, neurosurgeons at select U.S. hospitals have used 4K-3D extracorporeal video telescopes (exoscopes) to gain better visualization during brain surgery.¹ Now, an otolaryngologist at Penn State Health Milton S. Hershey Medical Center has found benefits to using this next-generation imaging technology to perform upper airway stimulation (UAS) surgery to treat obstructive sleep apnea (OSA).
Dr. Neerav Goyal, the Medical Center’s Chief, Division of Head and Neck Oncology and Surgery, performed a proof of concept study in 2019 evaluating the feasibility of using the ORBEYE 4K-3D exoscope during three consecutive UAS procedures.² All three cases were successfully completed, with no adverse events or complications, and the initial experience identified notable advantages over traditional approaches to UAS surgery.
For many patients with OSA, the first line of treatment is continuous positive airway pressure (CPAP) therapy. However, studies indicate that as many as 50% of patients prescribed CPAP either do not reach minimum adherence criteria or discontinue the treatment.³
UAS surgery is a relatively novel therapy designed for obstructive sleep apnea patients who cannot tolerate CPAP. Essential for the treatment is the precise placement of the cuff electrode around the select branches of the hypoglossal nerve that innervate the protrusors and stiffeners of the tongue. Another decisive step is the placement of the sensing lead between the intercostal muscles.4
Traditionally, surgeons perform UAS surgery using either surgical loupe magnification and/or binocular microscopy to identify those select hypoglossal nerve fibers. Goyal previously used a binocular microscope, and while it provided him the visualization he needed, “Only the people who look directly into the lens could see the surgical field,” Goyal says. “That meant the rest of the surgical team couldn’t see what I was seeing and anticipate the next steps of the surgery.”
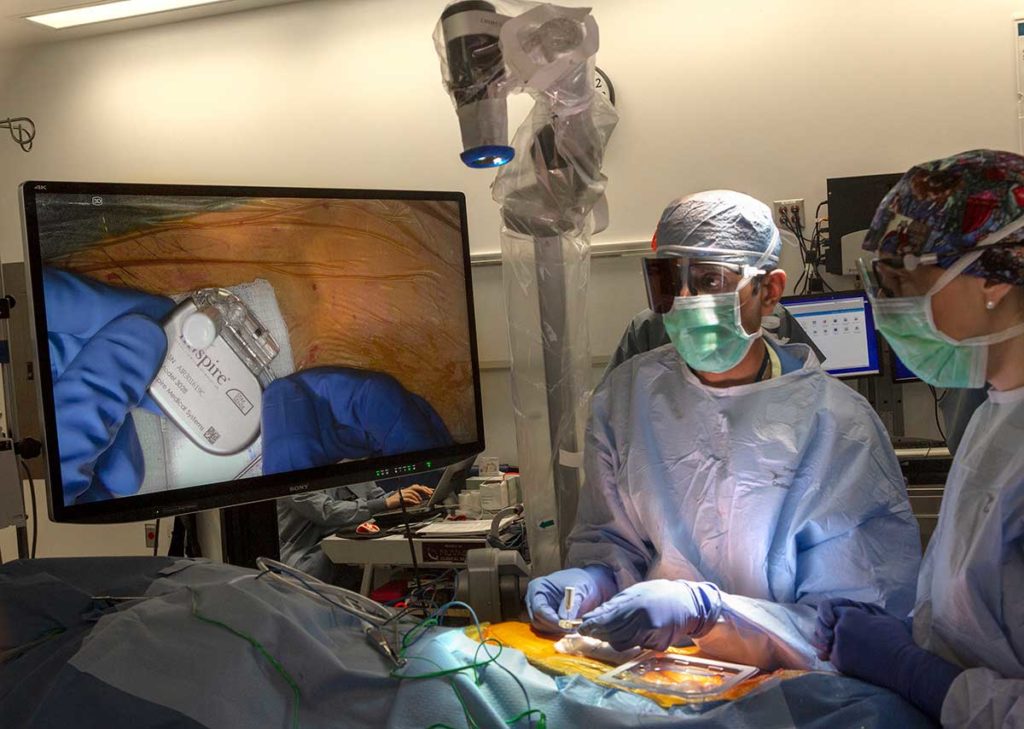
Dr. Neerav Goyal and a surgical team perform upper airway stimulation surgery using a 4K-3D exoscope.
Goyal noted the success Hershey Medical Center neurosurgeons had using the ORBEYE 4K-3D exoscope and envisioned its potential use for UAS procedures. “Our neurosurgeons work in a fixed space—inside the skull—and in UAS surgery, we also work in a fixed space—the area just underneath the neck,” Goyal says.
The exoscope, manufactured by Olympus America, includes a single articulating arm with a lens. Touch-sensitive controls allow the surgeon to change the lens focus, zoom or autofocus. During UAS surgery, the exoscope is suspended above the surgical field and produces a latency-free image. Its longer focal length (200 mm to 500 mm) allows for the entire system to be positioned farther from the surgical field, increasing the working corridor for surgeons.
Because the exoscope is about 50% smaller than microscopes previously used for UAS surgery, it allows surgeons to easily move from one view to another, improving ergonomics for the operating surgeon. In addition, the exoscope broadcasts 3D images to monitors within the operating room. “That allows everyone inside the OR—assistant surgeons, surgical technologists and nursing staff—to be on the same page, which improves communication and instrument exchange among team members,” Goyal says.
The 3D visualization also allows Goyal and his team to use it as a teaching platform, which is important in an academic medical setting such as Hershey Medical Center. “It allows the supervising surgeon to safely follow all aspects of the operation,” Goyal says.
During the proof of concept, all three UAS cases were successfully completed, with a mean operative time of 200 minutes (range 188 to 218 minutes) and reduction in operative time with consecutive usage of the exoscope. The mean operative time with the exoscope was slightly longer than published reports of 179 minutes with traditional microscopic technology.
Goyal states that otolaryngologic surgeons performing UAS with the exoscope could benefit from future studies providing a more systematic assessment of the device’s image quality, ergonomics and impact on surgical workflow.
“At Penn State Health, we’re always looking to leverage new technology to keep patients safe and allow us to do surgery more effectively,” Goyal says, “and the 4K-3D exoscope brings great promise to do just that for UAS patients.”

Neerav Goyal, MD, MPH, FACS
Chief, Division of Head and Neck Oncology and Surgery
Associate professor and vice chair for quality and safety, Department of Otolaryngology ─ Head and Neck Surgery
Associate professor, neurosurgery and public health sciences, Penn State College of Medicine
Phone: 717-531-6822
Email: ngoyal1@pennstatehealth.psu.edu
Fellowship: Surgical oncology, head and neck, Massachusetts Eye and Ear Infirmary, Harvard Medical School, Boston
Residency: Otolaryngology, and Otolaryngology – Head and Neck Surgery, Penn State Health Milton S. Hershey Medical Center
Medical School: Jefferson Medical College of Thomas Jefferson University, Philadelphia
Connect with Neerav Goyal, MD, MPH, FACS, on Doximity
References
- Grady D. Brain Surgery in 3-D: Coming Soon to the Operating Theater. The New York Times. Jan. 8, 2018. Accessed Sept. 25, 2020. nytimes.com
- Patel V, Goyal N. Using a 4K-3D Exoscope for Upper Airway Stimulation Surgery: Proof-of-Concept. Ann. Otol. Rhinol. Laryngol. 2020;129(7):695-698. doi: 10.1177/0003489420905873
- Pogach M. I can’t tolerate CPAP. What can I do? Harvard Health Blog. July 29, 2020. Accessed Sept. 25, 2020. health.harvard.edu/blog
- Heiser C, Thaler E, Boon M, Soose R, Woodson B. Updates of operative techniques for upper airway stimulation. Laryngoscope. 2016;126:S12-S16. doi: https://doi.org/10.1002/lary.26158

