Single-level laminectomy approach to selective dorsal rhizotomy improves outcomes for patients with spastic cerebral palsy
Spasticity, often regarded as the most common motor impairment in children with cerebral palsy, can bring difficulties to both patients and caregivers.1 Children with spastic cerebral palsy experience stiff muscles that can affect their gait patterns and make balance and movement challenging. Caregivers of children with the most severe levels of spasticity may find it nearly impossible to transfer them from a chair to a bed.
Historically, intrathecal baclofen pump therapy was the main treatment for spastic cerebral palsy. However, baclofen pumps carry the risk of both mechanical and infectious complications, and those complication rates are higher in children than adults.2
An alternative treatment, selective dorsal rhizotomy (SDR), is a well-established surgical procedure for improving lower extremity spasticity in children with cerebral palsy. Dr. S. Hassan Akbari, with Penn State Neuroscience Institute, is one of a select group of pediatric neurosurgeons in the nation performing SDR with a single-level laminectomy technique.
“For cerebral palsy patients who could benefit from improved ambulation, SDR can be a much better option than baclofen pump therapy, with a much lower risk profile,” Akbari says.
Akbari performed his residency in neurological surgery at Washington University in St. Louis School of Medicine, training under Dr. T.S. Park, who has performed more than 4,000 SDR surgeries.3 Park has also extensively published on SDR, including a co-authored study that showed 95% of adult patients who received SDR in childhood reported positive effects on quality of life and ambulation 20 to 28 years later.4
The single-level laminectomy approach to SDR is unique in that it removes a single piece of bone, as opposed to multilevel techniques to SDR that remove multiple levels of bone. “The single-level laminectomy approach is less invasive,” Akbari says. “Here at Penn State Health Children’s Hospital, we reattach the bone as well, and this, coupled with the limited bony removal, decreases the risk for spinal column deformities down the road.
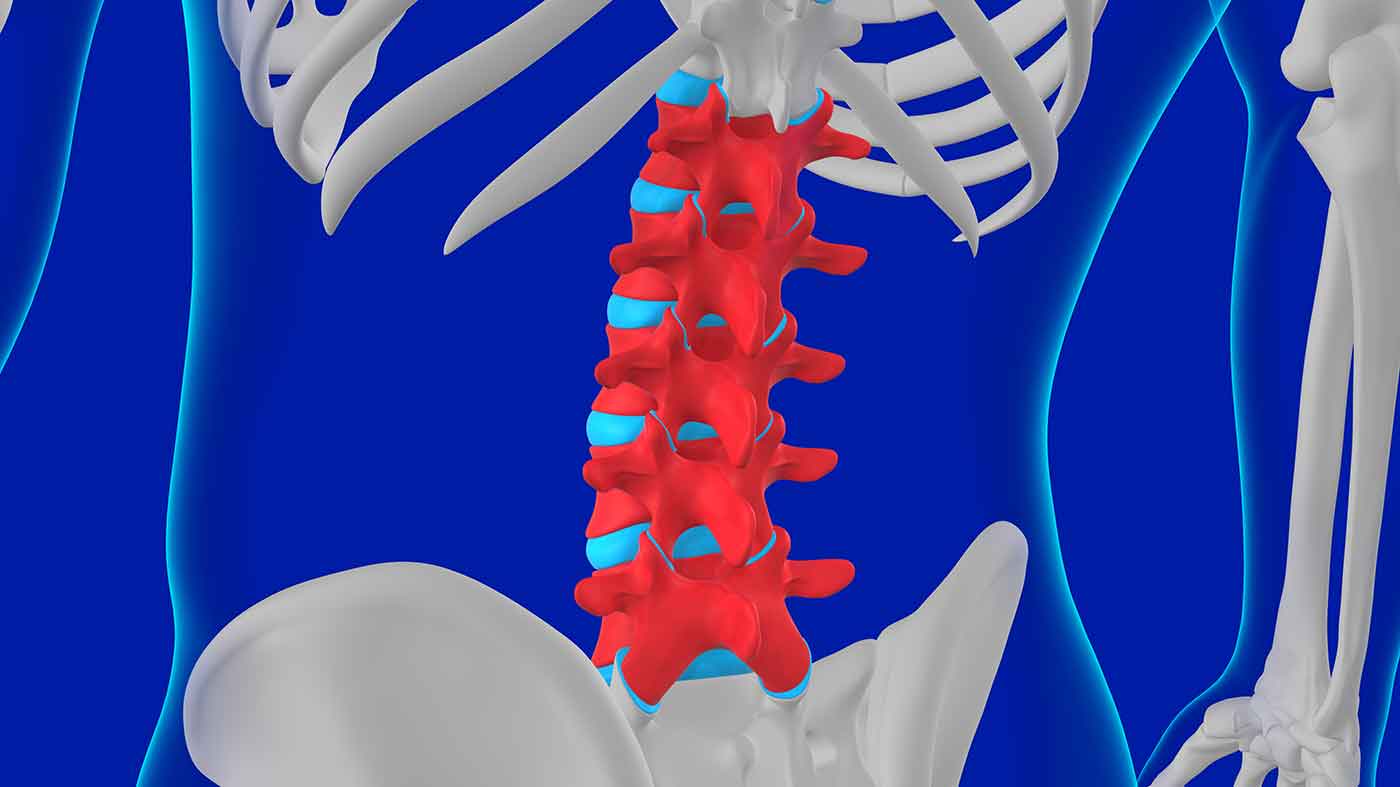
SDR is typically performed for rootlets between spinal nerves L1 and S1/S2.
During an SDR at the Children’s Hospital, Akbari uses a preoperative MRI to identify the level where the spinal cord terminates before sending nerve roots to the lower extremities. “We make an incision at that level, remove the back part of a single piece of bone, move it to the side, and then open up the lining around the nerve roots to gain access to them,” Akbari says.
Akbari then uses electromyography and somatosensory evoked potentials to evaluate the nerve roots, splitting each into three nerve rootlets, and sectioning the two rootlets with the most abnormal firing pattern. “We then repeat that process for each of the nerve roots on the right and left side.” Once the misfiring nerve roots are severed, Akbari replaces the cut piece of bone with a suture and closes the patient. The procedure typically takes between four to five hours.
Patients typically stay in the hospital for five days, then proceed to inpatient rehabilitation for four to six weeks of physical and occupational therapy. Local patients can receive inpatient therapy at Penn State Health Rehabilitation Hospital in Hershey, Pa., under the supervision of Dr. Teresa Such-Neibar, medical director of the Pediatric Rehabilitation Program at Penn State Health Children’s Hospital. The Children’s Hospital also has relationships with other rehabilitation hospitals for patients who live outside of central Pennsylvania.
“The goal of SDR is to bring patients up at least one level in terms of their mobility,” Akbari says. For example, patients who use a walker to ambulate may be able to use canes or crutches after SDR. Those on crutches prior to an SDR may be able to walk with limited assistance afterward. Those who walk with an abnormal gait pattern may be able to walk more normally following SDR.
SDR can be used to treat both spastic diplegia (spasticity affecting only the lower extremities) and spastic quadriplegia (spasticity affecting both the lower and upper extremities). The best candidates are patients who are at least 4 years old and have a level of spasticity that causes problems in day-to-day care and functioning.
Akbari also performs the rhizotomy procedure for patients with the most severe cases of spasticity. This procedure, termed a palliative rhizotomy, is similar to SDR but also includes the selective sectioning of ventral nerve roots responsible for motor movement. “This helps release a patient’s muscles further so they’re not as tight,” Akbari says. Palliative rhizotomy is reserved for patients who are at risk for fractures or dislocations due to spasticity, or patients who can’t release their legs during transfer from a chair to a bed. This procedure also helps caregivers care for their child by releasing the severe tone, allowing for better patient hygiene and care.
“Throughout our region, we have a very large cohort of patients with cerebral palsy and spasticity,” Akbari says. “These types of surgeries can help them reduce muscle tone and gain mobility.”
References
- Bar-On L, Molenaers G, Aertbeliën E, et al. Spasticity and its contribution to hypertonia in cerebral palsy. Biomed Res Int. 2015;2015:317047. doi:10.1155/2015/317047
- Woolf SM, Baum CR. Baclofen Pumps: Uses and Complications. Pediatr Emerg Care. 2017;33(4):271-275. doi:10.1097/PEC.0000000000001090
- McGrath P. Number 4,000 – Dr. Park reaches an SDR surgical milestone. St. Louis Children’s Hospital Website. https://www.stlouischildrens.org/health-resources/pulse/number-4000-dr-park-reaches-sdr-surgical-milestone. Published November 2018. Accessed January 12, 2022.
- Park TS, Liu JL, Edwards C, Walter DM, Dobbs MB. Functional Outcomes of Childhood Selective Dorsal Rhizotomy 20 to 28 Years Later. Cureus. 2017 May 17;9(5):e1256. doi: 10.7759/cureus.1256. PMID: 28649479; PMCID: PMC5473717.
