Blood Pressure Management May Play Key Role in Ischemic Stroke Recovery Following Mechanical Thrombectomy
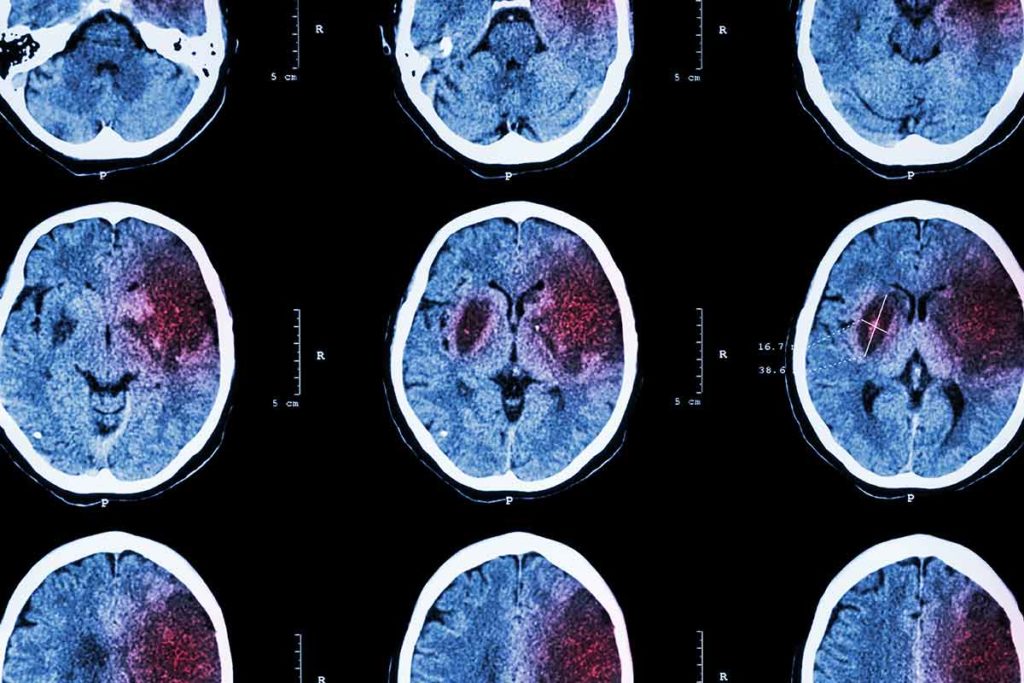
Since the first clot retrieval device received U.S. Food and Drug administration approval in 2004, mechanical thrombectomy has emerged as a standard treatment for large vessel ischemic stroke.¹ While its efficacy is proven, less is known about how to best manage blood pressure in patients following successful mechanical thrombectomy. To find an answer, a team of researchers from Penn State Health Stroke Center and the Department of Neurosurgery at Penn State Health Milton S. Hershey Medical Center performed a retrospective study of 117 adult acute ischemic stroke patients who underwent mechanical thrombectomy. The results indicate that individual instances of elevated systolic blood pressure (SBP) can significantly affect clinical outcomes.²
“The study showed us that, even if a patient has blood flow restored through mechanical thrombectomy, blood pressure control is still important post-surgery,” said Neurosurgeon Dr. Kevin Cockroft, a co-author of the study and new interim chair of the Department of Neurosurgery.
Researchers collected SBP data for the first 24 hours following mechanical thrombectomy. They then categorized the patients into three groups according to cases of SBP above 140, 160 or 180 mm Hg.
“We were particularly interested in instances of high blood pressure rather than average blood pressure over time because we weren’t convinced average blood pressure was a good measure of the problem,” Cockroft said.
The team used the modified Rankin Scale to determine patients’ functional outcomes at 90 days. The team also measured patient mortality, cerebral edema and rate of hemorrhage during their first 90 days in recovery.
The Penn State Health Stroke Center team performs about 100 mechanical thrombectomies on acute ischemic stroke patients each year.
The results showed that just one instance of SBP exceeding 180 mm Hg was significantly associated with poor functional outcomes at discharge but not at 90 days post follow-up.
“Over time, we found the levels of recovery started to converge regardless of a patient’s blood pressure,” Cockroft said. “However, that doesn’t indicate whether patients with one instance of elevated SBP will need more time in rehabilitation or other treatment to make an optimal recovery.” The study also found that one or more occurrence of SBP over 160 mm Hg resulted in increased odds of malignant cerebral edema, with a trend toward increased odds of symptomatic intracranial hemorrhage. These findings were independent of stroke severity.
“The results emphasize the importance of medical and nursing staff providing frequent and accurate blood pressure monitoring for patients after mechanical thrombectomy and responding to instances of high blood pressure with the appropriate medication,” Cockroft said.
A potential next step for researchers is to look at prospective trials that could measure the influence of blood pressure management in these patients. “Our study was limited in that we had a relatively small number of patients,” Cockroft said.
Cockroft’s co-authors were neurosurgery residents Dr. Michael Gigliotti and Dr. Varun Padmanaban; clinical nurse specialist and Stroke Program manager Alicia Richardson; and neurosurgeons Dr. Scott Simon and Dr. Ephraim Church.
The Penn State Health Stroke Center is one of only seven health care facilities in Pennsylvania—and the first one in central Pennsylvania—to achieve status as a certified Comprehensive Stroke Center by The Joint Commission and the American Heart Association/American Stroke Association.
The Stroke Center’s team cares for about 1,000 stroke cases each year, roughly 60% to 70% of which are acute ischemic strokes. The team performs about 100 mechanical thrombectomies each year and invests in research to improve the care of stroke patients and raise awareness of stroke throughout the community.

Kevin M. Cockroft, MD, MSc, FAANS, FACS, FAHA
Co-Director, Penn State Health Stroke Center
Interim Chair, Department of Neurosurgery, Penn State College of Medicine
Professor, Departments of Neurosurgery, Radiology and Public Health Sciences
Phone: 717-531-3828
Email: kcockroft@pennstatehealth.psu.edu
Fellowship: Interventional/Vascular, Thomas Jefferson University Hospital, Philadelphia, Pa.; Neurological Surgery, Stanford University Hospital, Stanford, Calif.
Residency: Neurological Surgery, The New York Hospital-Cornell Medical Center, New York, N.Y.
Medical School: Cornell University Medical College, New York, N.Y.
Connect with Kevin M. Cockroft, MD, MSc, FAANS, FACS, FAHA, on Doximity
References
- Smith WS, Furlan AJ. Brief History of Endovascular Acute Ischemic Stroke Treatment. Stroke. 2016;47(2):e23-e26. doi:10.1161/STROKEAHA.115.010863
- Gigliotti MJ, Padmanaban V, Richardson A, Simon SD, Church EW, Cockroft KM. Effect of Blood Pressure Management Strategies on Outcomes in Patients with Acute Ischemic Stroke After Successful Mechanical Thrombectomy. World Neurosurg. 2021 Apr;148:e635-e642. doi: 10.1016/j.wneu.2021.01.052
